Are you doing all the “right” things but still find your Insulin levels up?
The connection between insulin resistance and perimenopause is an important area of research, particularly as women transition through this phase and experience hormonal changes that can impact metabolic health.
Dr. Ben Bikman and other researchers have explored how these changes can influence insulin sensitivity and contribute to various health issues.
Here are the key points explaining this connection:
Hormonal Changes During Perimenopause
- Decline in Estrogen:
- Estrogen’s Role: Estrogen has a protective effect on insulin sensitivity. It helps to regulate glucose and lipid metabolism and influences fat distribution.
- Impact of Decline: As estrogen levels decline during perimenopause, women may experience decreased insulin sensitivity. This decline can contribute to increased visceral fat accumulation and a higher risk of insulin resistance.
- Changes in Progesterone:
- Progesterone’s Role: Progesterone also plays a role in metabolism and insulin sensitivity, although its effects are less pronounced than estrogen.
- Fluctuating Levels: During perimenopause, progesterone levels can fluctuate significantly, potentially contributing to metabolic instability and changes in insulin sensitivity.
Metabolic and Physiological Effects
- Weight Gain and Fat Distribution:
- Increased Visceral Fat: The decline in estrogen often leads to a shift in fat distribution, with an increase in visceral fat (abdominal fat), which is more strongly associated with insulin resistance.
- Overall Weight Gain: Many women experience weight gain during perimenopause, partly due to hormonal changes and decreased metabolic rate.
- Inflammation:
- Increased Inflammation: Declining estrogen levels are associated with increased systemic inflammation. Inflammation can interfere with insulin signaling pathways, exacerbating insulin resistance.
- Chronic Low-Grade Inflammation: This type of inflammation is commonly seen in both insulin resistance and menopausal transition.
- Muscle Mass and Physical Activity:
- Loss of Muscle Mass: Aging and hormonal changes can lead to a decline in muscle mass, which is important for maintaining insulin sensitivity.
- Decreased Physical Activity: Many women reduce their physical activity levels during perimenopause, contributing to weight gain and insulin resistance.
Strategies to Mitigate Insulin Resistance During Perimenopause
- Dietary Changes:
- Low-Carbohydrate Diets: Reducing carbohydrate intake can help manage blood glucose levels and improve insulin sensitivity.
- Anti-Inflammatory Foods: Incorporating foods that reduce inflammation, such as omega-3 fatty acids, leafy greens, and berries, can be beneficial.
- Regular Physical Activity:
- Strength Training: Resistance training can help maintain and build muscle mass, which improves insulin sensitivity.
- Aerobic Exercise: Regular aerobic exercise helps improve overall metabolic health and insulin sensitivity.
- Weight Management:
- Healthy Weight: Maintaining a healthy weight through balanced diet and exercise is crucial for managing insulin resistance.
- Hormone Replacement Therapy (HRT):
- Potential Benefits: Some women may benefit from HRT, which can help mitigate the decline in estrogen and its associated effects on insulin sensitivity and fat distribution. However, HRT should be discussed with a healthcare provider to weigh potential risks and benefits.
- Stress Management and Sleep:
- Reducing Stress: Chronic stress can increase cortisol levels, which negatively affect insulin sensitivity.
- Adequate Sleep: Ensuring sufficient and quality sleep is essential for metabolic health.
Summary
The connection between insulin resistance and perimenopause is multifaceted, involving hormonal changes, shifts in fat distribution, inflammation, and lifestyle factors. Declining estrogen and fluctuating progesterone levels during perimenopause can lead to decreased insulin sensitivity and increased visceral fat, contributing to insulin resistance. Addressing these issues through diet, exercise, weight management, and potentially hormone replacement therapy can help mitigate the impact of perimenopause on insulin resistance and overall metabolic health.
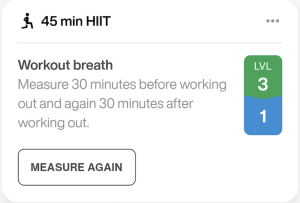
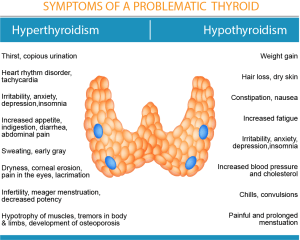
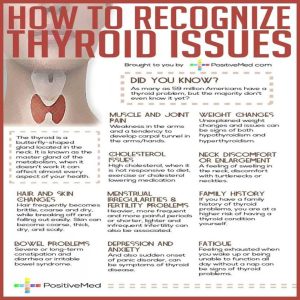
Do you have Low Thyroid + Low Cortisol + Insulin Resistance??
Low thyroid function, also known as hypothyroidism, can significantly impact glucose metabolism in several ways due to the critical role thyroid hormones play in regulating various metabolic processes.
Here’s a detailed explanation:
Slowed Glucose Absorption in Cells:
-
- Thyroid hormones (primarily T3 and T4) are crucial for the regulation of cellular metabolism, including the uptake and utilization of glucose by cells.
- In hypothyroidism, the reduced levels of these hormones lead to decreased cellular metabolism, which means cells absorb glucose more slowly.
This slower absorption can result in higher blood glucose levels, as glucose remains in the bloodstream rather than being taken up by cells for energy production.
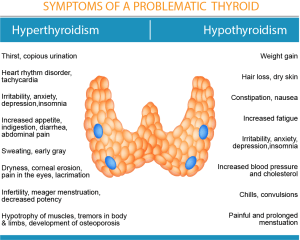
Hindered Gut Glucose Absorption
-
- Thyroid hormones also influence the gastrointestinal tract’s function.
- In cases of low thyroid function, gastrointestinal motility can be reduced, meaning that the movement of food and nutrients through the digestive system is slower.
- This reduced motility can lead to impaired absorption of glucose from the gut into the bloodstream, contributing to irregular blood glucose levels.
Slowed Pancreatic Response:
-
-
- The pancreas plays a vital role in glucose metabolism by producing insulin, which helps regulate blood glucose levels.
- Thyroid hormones affect the pancreas’s ability to respond to blood glucose levels and produce insulin efficiently.
- Hypothyroidism can slow down the pancreatic response, meaning insulin release is less timely and less effective, leading to potential dysregulation of blood glucose levels.
Decreased Insulin Clearance: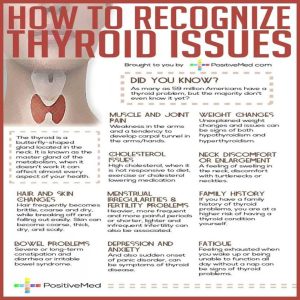
-
- Insulin clearance refers to the process by which insulin is removed from the bloodstream, primarily by the liver and kidneys.
- Thyroid hormones influence the metabolic activity of the liver, including its ability to clear insulin from the blood.
- In hypothyroidism, the reduced thyroid hormone levels can decrease the liver’s efficiency in clearing insulin, resulting in prolonged insulin presence in the bloodstream.
- This prolonged presence can contribute to insulin resistance, where cells become less responsive to insulin, further complicating glucose regulation.
Overall, the interplay between thyroid hormones and glucose metabolism is complex. When thyroid function is low, it disrupts multiple processes involved in maintaining normal blood glucose levels, which can contribute to conditions like hyperglycemia (high blood sugar) and increase the risk of developing insulin resistance and type 2 diabetes. Proper management of hypothyroidism through medication and lifestyle adjustments can help mitigate these effects and improve glucose metabolism
WHY does elevated insulin cause weight gain?
Elevated insulin levels can significantly influence fat storage and inhibit fat breakdown, making weight loss challenging due to several physiological mechanisms:
1. Promotes Fat Storage (Lipogenesis)
- Stimulates Adipocytes: Insulin stimulates adipocytes (fat cells) to absorb glucose from the bloodstream. Once inside the adipocytes, glucose is converted into triglycerides (fat molecules) for storage.
- Activates Lipogenic Enzymes: Insulin activates enzymes like acetyl-CoA carboxylase and fatty acid synthase, which are crucial for the synthesis of fatty acids and triglycerides.
- Inhibits Lipolysis: Insulin inhibits hormone-sensitive lipase (HSL), an enzyme responsible for breaking down stored triglycerides into free fatty acids, thus reducing the release of fatty acids from fat stores.
2. Inhibits Fat Breakdown (Lipolysis)
- Reduces Hormone-Sensitive Lipase Activity: As mentioned, insulin suppresses HSL, thereby decreasing the breakdown of stored fat.
- Promotes Re-esterification: Insulin promotes the re-esterification of free fatty acids back into triglycerides within adipocytes, further enhancing fat storage and preventing the use of fatty acids as an energy source.
3. Alters Energy Utilization
- Preferential Glucose Utilization: Elevated insulin levels shift the body’s energy utilization preference towards glucose rather than fat. When insulin is high, cells primarily use glucose for energy, which reduces the oxidation of fatty acids.
- Reduces Ketogenesis: Insulin inhibits ketogenesis in the liver. Ketogenesis is the process of producing ketone bodies from fatty acids, which can be used as an alternative energy source when glucose is scarce.
4. Regulates Appetite and Satiety
- Impacts on Hunger Hormones: Insulin can influence other hormones involved in hunger and satiety, such as ghrelin (hunger hormone) and leptin (satiety hormone). Dysregulation in these hormones can lead to increased appetite and calorie intake.
- Insulin Resistance: Chronic high insulin levels can lead to insulin resistance, where the body’s cells become less responsive to insulin. This condition is often associated with increased hunger and higher fat accumulation, creating a vicious cycle.
5. Metabolic Implications
- Insulin and Metabolic Rate: Insulin affects basal metabolic rate (BMR) by influencing thyroid hormones and other metabolic regulators. High insulin levels can lead to a decrease in BMR, making it harder to burn calories efficiently.
- Glycogen Storage: Insulin promotes the storage of excess glucose as glycogen in the liver and muscles. Once glycogen stores are full, additional glucose is converted to fat, contributing to weight gain.
6. Interference with Fat Mobilization
- Impaired Mobilization of Fat: With high insulin levels, the body has a harder time mobilizing and using fat stores for energy, leading to persistent fat accumulation even with calorie restriction or exercise.
In summary, elevated insulin levels create an environment that favors fat storage and inhibits fat breakdown through multiple biochemical and hormonal pathways. This makes it challenging to lose weight, as the body is primed to store excess calories as fat and use glucose as the primary energy source, thereby hindering effective fat loss.
Do you struggle with metabolic INFLEXIBILITY?
Both Dr. Ben Bikman and Dr. Stacy Sims discuss the interconnectedness of insulin resistance, chronic stress, weight gain, peri-menopause, and metabolic inflexibility, albeit from slightly different perspectives due to their distinct areas of expertise.
Dr. Ben Bikman
1. Insulin Resistance: Dr. Bikman focuses extensively on insulin resistance as a central factor in metabolic health. He explains that insulin resistance, where cells become less responsive to insulin, leads to elevated blood glucose levels and increased insulin production. This can cause a cascade of metabolic issues.
2. Chronic Stress: Chronic stress contributes to insulin resistance. Stress hormones like cortisol can increase blood sugar levels, which in turn, can prompt higher insulin secretion. Over time, this can exacerbate insulin resistance.
3. Weight Gain: Insulin resistance often leads to weight gain, especially around the abdomen. Elevated insulin levels promote fat storage and inhibit fat breakdown, making weight loss challenging.
4. Peri-Menopause: During peri-menopause, hormonal changes (e.g., decreased estrogen levels) can exacerbate insulin resistance. Estrogen helps modulate insulin sensitivity, and its decline can lead to increased fat accumulation and metabolic disturbances.
5. Metabolic Inflexibility: Insulin resistance is closely linked to metabolic inflexibility, the reduced ability to switch between burning carbohydrates and fats for energy. This inflexibility can result in a reliance on carbohydrates for energy, further worsening insulin resistance and weight gain.
Dr. Stacy Sims
1. Insulin Resistance: Dr. Sims also recognizes the role of insulin resistance but often emphasizes its interaction with female physiology, particularly during different life stages such as peri-menopause.
2. Chronic Stress: Dr. Sims highlights how chronic stress impacts women differently, particularly through the hormonal changes experienced during peri-menopause. Increased cortisol levels from stress can lead to insulin resistance and weight gain.
3. Weight Gain: She notes that weight gain during peri-menopause is common and often exacerbated by insulin resistance. This weight gain tends to be more visceral (around the organs), which is more metabolically active and problematic.
4. Peri-Menopause: Dr. Sims focuses on how hormonal fluctuations during peri-menopause, including decreases in estrogen and progesterone, influence metabolic processes. These changes can lead to increased insulin resistance, weight gain, and changes in body composition.
5. Metabolic Inflexibility: Dr. Sims discusses metabolic inflexibility in the context of how women’s bodies adapt to different hormonal states. During peri-menopause, reduced estrogen levels can make it harder for the body to efficiently switch between fuel sources, leading to a propensity for weight gain and difficulty in losing weight.
Synthesis of Perspectives
Common Ground: Both Dr. Bikman and Dr. Sims agree that insulin resistance is a pivotal issue that links chronic stress, weight gain, peri-menopause, and metabolic inflexibility. They both emphasize the detrimental impact of chronic stress and hormonal changes on metabolic health.
Unique Insights:
- Dr. Bikman delves deeply into the biochemical pathways of insulin resistance and how it contributes to broader metabolic syndrome.
- Dr. Sims provides a nuanced view of how female hormonal changes, particularly during peri-menopause, specifically affect metabolic health and insulin sensitivity.
Conclusion: The relationship between insulin resistance, chronic stress, weight gain, peri-menopause, and metabolic inflexibility is complex and interdependent. Managing insulin resistance through lifestyle interventions (e.g., diet, exercise, stress management) is crucial, especially for women undergoing peri-menopause, to maintain metabolic health and prevent weight gain. Both experts provide valuable insights into how these factors interplay and impact overall health.
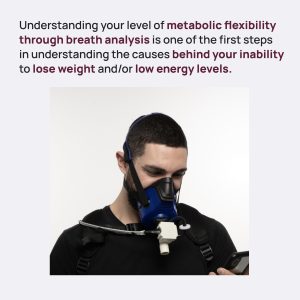
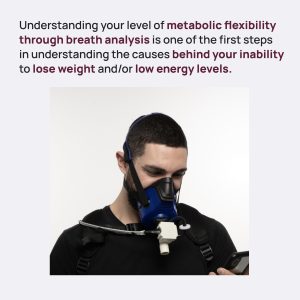
LUMEN: Test and not Guess your Fat or Carb Burn
Abstract

Metabolic carts measure the carbon dioxide (CO2) produced and oxygen consumed by an individual when breathing to assess metabolic fuel usage (carbohydrates versus fats). However, these systems are expensive, time-consuming, and only available in health care laboratory settings. A small handheld device capable of determining metabolic fuel usage via CO2 from exhaled air has been developed.
Objective:
The aim of this study is to evaluate the validity of a novel handheld device (Lumen) for measuring metabolic fuel utilization in healthy young adults.
Methods:
- Metabolic fuel usage was assessed in healthy participants (n=33; mean age 23.1 years, SD 3.9 years) via respiratory exchange ratio (RER) values obtained from a metabolic cart as well as % CO2 from the Lumen device.
- Measurements were performed at rest in two conditions: fasting, and after consuming 150 grams of glucose, in order to determine changes in metabolic fuel usage.
- Reduced major axis regression and simple linear regression were performed to test for agreement between RER and Lumen % CO2.
Results:
- Both RER and Lumen % CO2 significantly increased after glucose intake (P<.001 for both) compared with fasting conditions, by 0.089 and 0.28, respectively.
- Regression analyses revealed an agreement between the two measurements (F1,63=18.54; P<.001).
Conclusions:
- This study shows the validity of Lumen for detecting changes in metabolic fuel utilization in a comparable manner with a laboratory standard metabolic cart, providing the ability for real-time metabolic information for users under any circumstances.
Interact J Med Res 2021;10(2):e25371
https://www.i-jmr.org/2021/2/e25371
Solutions for improving Insulin Sensitivity & Hormone Balance as we Age!?
Improving metabolic health, metabolic flexibility, and insulin sensitivity during peri-menopause and post-menopause involves a multi-faceted approach that includes lifestyle changes, dietary adjustments, physical activity, stress management, and possibly medical interventions. Here are detailed strategies based on expert recommendations:
1. Dietary Adjustments
1.1. Balanced Diet:
- Increase Protein Intake: Protein supports muscle maintenance and can improve satiety, which helps manage weight.
- Healthy Fats: Include sources of omega-3 fatty acids (e.g., fish, flaxseeds) which can help reduce inflammation and improve insulin sensitivity.
- Fiber-Rich Foods: May help improve gut health and manage blood sugar levels.
1.2. Carbohydrate Management:
- Low Glycemic Index Foods: Choose carbohydrates that have a lower impact on blood sugar levels
- Reduce Refined Carbohydrates: Minimize intake of sugary snacks, white bread, and other refined carbs that spike blood sugar levels.
1.3. Intermittent Fasting:
- Consider incorporating intermittent fasting or time-restricted eating, which can improve insulin sensitivity and promote metabolic flexibility.
2. Physical Activity
2.1. Strength Training:
- Resistance Exercises: Engaging in regular strength training (e.g., weightlifting, bodyweight exercises) helps maintain muscle mass, which is crucial for metabolic health and insulin sensitivity.
2.2. Aerobic Exercise:
- Cardio Activities: Regular aerobic exercise (e.g., walking, running, cycling) improves cardiovascular health and helps manage weight.
2.3. High-Intensity Interval Training (HIIT):
- HIIT Workouts: Short bursts of intense exercise followed by recovery periods can be particularly effective in improving metabolic flexibility and insulin sensitivity.
3. Stress Management
3.1. Mindfulness Practices:
- Meditation and Yoga: Practices such as mindfulness meditation, yoga, and deep breathing exercises can help reduce chronic stress and lower cortisol levels.
3.2. Adequate Sleep:
- Improve Sleep Hygiene: Ensure regular sleep patterns, avoid screens before bed, and create a restful environment to support better sleep, which is crucial for metabolic health.
4. Hormonal Support
4.1. Hormone Replacement Therapy (HRT):
- Consult a Healthcare Provider: For some women, HRT can help manage the symptoms of menopause, including its impact on metabolic health. Discuss the risks and benefits with a healthcare provider.
4.2. Natural Supplements:
- Consider Supplements: Supplements such as omega-3 fatty acids, vitamin D, and magnesium may support metabolic health. Always consult with a healthcare provider before starting new supplements.
5. Lifestyle Modifications
5.1. Avoid Smoking and Limit Alcohol:
- Healthy Habits: Smoking cessation and moderating alcohol consumption can significantly improve overall health and metabolic function.
5.2. Hydration:
- Stay Hydrated: Adequate water intake is essential for metabolic processes and overall health.
6. Regular Health Monitoring
6.1. Regular Check-Ups:
- Monitor Health Markers: Regularly check blood sugar levels, lipid profiles, and other metabolic markers with your healthcare provider to keep track of your progress and adjust strategies as needed.
Expert-Specific Recommendations
Dr. Ben Bikman:
- Low-Carbohydrate Diets: Dr. Bikman often recommends a low-carb or ketogenic diet to improve insulin sensitivity and metabolic health.
- Regular Fasting: He supports intermittent fasting as a tool to improve metabolic flexibility and manage insulin levels.
Dr. Stacy Sims:
- Nutrition Tailored for Women: Dr. Sims emphasizes the importance of nutrition that is specifically tailored to women’s unique hormonal and physiological needs, particularly during peri-menopause and post-menopause.
- Adaptation of Exercise Regimens: She recommends adjusting exercise routines to align with hormonal fluctuations, such as incorporating more strength training and less high-intensity cardio during certain phases.
Conclusion
Improving metabolic health, flexibility, and insulin sensitivity in peri-menopausal and post-menopausal women involves a comprehensive approach that includes a balanced diet, regular physical activity, stress management, adequate sleep, and regular health monitoring. Tailoring these strategies to individual needs and possibly incorporating expert-specific recommendations from professionals like Dr. Ben Bikman and Dr. Stacy Sims can help manage the metabolic challenges associated with aging and hormonal changes.
Do you want a Personalized Coaching Program?
Just ask me for a consultation to learn more about how I help you live your best life in your second half of your life- so you can thrive as you age.
I wanted to share a new additional service I am implementing into my The WHOLESTIC Method online coaching program to help you learn how to be more metabolically flexible as it has a wealth of benefits!.
Now available with my The WHOLESTIC Method Coaching program, we are offering access to Lumen, a metabolic device you can bring with you anywhere that is helping our clients achieve weight loss, enhance athletic performance and improve overall metabolic health.
The beauty of metabolic flexibility is that it’s not a fixed trait; research shows that a flexible metabolism can improve your overall health through changes in your lifestyle like regular exercise, and quality sleep. Follow your nutrition plan each day to improve your metabolic flexibility and keep track of your progress by taking morning measurements.
Good metabolic flexibility allows your body to efficiently switch between different fuel sources for energy, including stored fat. As a result, this can make it easier to lose weight and achieve optimal body composition.
Greater Energy Levels
With good metabolic flexibility, you may experience more stable and greater energy levels throughout the day and have an easier time maintaining your energy levels during prolonged exercise and physical activity.
Plan When to Eat Your Carbs from Nature
Developing good metabolic flexibility may help to prevent chronic diseases and support long-term health and well-being, allowing you to enjoy a healthier, happier life.
Remember that everyone’s journey is different, and your metabolism and nutrition needs are unique, which is why your personalized nutrition plan is crucial to achieving your goals.
The best part about it – we can help by monitoring your data! Purchasing a Lumen through The WHOLIESTIC Method- Debbie Potts Coaching program will allow you to opt into additional coaching sessions. Let our team support you and guide you through your metabolic journey. Ask me about my packages as low as $297 per month: The Assessment, The Accountability Package, The Health Investigation or The Longevity VIP monthly packages to get your unique personalized coaching program.
Take care of the WHOLE you from the inside out!
More details on my website and YouTube Channel
Dihydroberberine SR:
GlucoVantage® dihydroberberine as a sustained-release dietary supplement, offers several potential benefits based on scientific research:
- Improved Blood Glucose Control: Berberine, the active component in dihydroberberine, has been extensively studied for its ability to improve insulin sensitivity and reduce blood glucose levels. Research suggests that berberine can be effective in managing blood sugar levels in individuals with insulin resistance or type 2 diabetes.
- Enhanced Insulin Sensitivity: Berberine has been shown to activate AMP-activated protein kinase (AMPK), an enzyme that plays a key role in regulating cellular energy metabolism. By activating AMPK, berberine may enhance insulin sensitivity, which can help in better glucose uptake by cells and improved metabolic health.
- Support for Weight Management: Studies have indicated that berberine may help in weight management by influencing various metabolic pathways. It can potentially reduce fat accumulation, especially visceral fat, and may aid in controlling appetite and food intake.
- Cardiovascular Health: Berberine has shown promise in supporting cardiovascular health by helping to regulate lipid levels, including reducing LDL cholesterol and triglycerides while increasing HDL cholesterol. These effects contribute to a healthier lipid profile and may reduce the risk of cardiovascular diseases.
- Anti-inflammatory Properties: Berberine exhibits anti-inflammatory effects, which can be beneficial for overall health. Chronic inflammation is linked to various diseases, and reducing inflammation markers can have a positive impact on health outcomes.
- Liver Health: Berberine has been studied for its potential to support liver health by improving liver function and reducing fatty liver disease. This is particularly important for individuals with metabolic syndrome or non-alcoholic fatty liver disease (NAFLD).
- Gut Health: Berberine may also support gut health by modulating gut microbiota composition and improving intestinal barrier function. A healthy gut microbiome is crucial for overall digestion, nutrient absorption, and immune function.
- Antioxidant Properties: Berberine exhibits antioxidant activity, which helps in combating oxidative stress and reducing cellular damage caused by free radicals. This antioxidant effect contributes to its overall health benefits.
- Bioavailability: Dihydroberberine, the form used in GlucoVantage®, is reported to have higher bioavailability than traditional berberine. This means it can potentially offer greater effectiveness at lower doses, reducing the risk of gastrointestinal side effects that can occur with higher doses of regular berberine.
It’s important to note that while the benefits of dihydroberberine and berberine are supported by scientific research, individual responses may vary. It’s always advisable to consult with a healthcare professional before starting any new supplement regimen, especially if you have pre-existing medical conditions or are taking medications.
7 Promising Uses of Berberine
One of the most compelling features of berberine is its wide application to treat a number of health problems, including cardiovascular and metabolic diseases (CVMD). CVMD includes heart conditions like heart failure, hypertension (high blood pressure), and atherosclerosis, to name just a few. It also includes metabolic diseases like obesity, diabetes, and non-alcoholic fatty liver disease.⁴ These diseases are some of the leading causes of death worldwide.⁷
Berberine has a strong clinical and safety profile and considerable pharmacological research to support its use.⁴
So, how does it combat these diseases and optimize your health?
To start, berberine is a glucose disposal agent, which means it lowers blood sugar levels through nutrient partitioning.
Nutrient partitioning is the process of pushing more glucose into the muscle than fat through the help of AMP-activated protein kinase, or AMPK.
As a result, berberine:
- Reduces insulin resistance
- Promotes fat loss
- Helps with growth hormone potentiation
- Leads to longer telomeres
- Is anti-aging (by reducing advanced glycation end-products (AGEs), which is blood sugar damage)
- Improves mitochondrial functioning
- Improves with gut microbes
- Raises ketones
It is an effective and powerful supplement!
Because of these health-optimizing and disease-healing properties, berberine is often used to treat these health problems:
Diabetes
Berberine is perhaps best known for its effectiveness in treating diabetes. The main way it does this is by reducing blood sugar. It is sometimes called an “insulin sensitizer” because it reduces insulin resistance. Metformin and rosiglitazone are two common pharmaceutical drugs used to help regulate blood sugar in individuals with diabetes. Taking 500 mg of berberine 2-3 times per day has been shown to be as effective as both of these two prescription drugs.
Cholesterol
High cholesterol is a major risk factor for heart disease that affects about ⅓ of the US population.8 There are several ways to lower your cholesterol, including important lifestyle changes like eating heart-healthy foods, exercising regularly, quitting smoking, losing weight, and reducing your alcohol intake.
Berberine is another excellent tool for reducing cholesterol – it has been shown to reduce total cholesterol, lipoprotein (LDL or “bad”) cholesterol, and triglycerides.6 In fact, multiple studies show that it is as effective as standard prescription medications for lowering cholesterol and may be more effective than standard prescription drugs at reducing triglycerides.⁸ When your triglycerides are too high, you are at greater risk for heart disease and stroke.
High Blood Pressure
Berberine can help increase the effectiveness of blood pressure medications when it is used alongside these medications in individuals with high blood pressure. For example, taking berberine with amlodipine, a common blood pressure medication, reduces both systolic and diastolic blood pressure better than taking amlodipine alone.
As is the case with many of these health conditions, lifestyle factors play an important role in improving health and reducing symptoms of disease. Other ways to improve blood pressure include⁹:
-
- Exercise – aim for 150 minutes of exercise per week, or about 30 minutes per day, 5 days per week
- Lose weight if you are overweight
- Reduce sugar intake
- Reduce sodium and increase potassium intake
- Quit smoking
- Limit your stress
- Reduce alcohol and caffeine intake
Polycystic Ovary Syndrome (PCOS)
In recent years, berberine has been used to help treat a common hormonal disorder in women called polycystic ovary syndrome, or PCOS. PCOS can cause enlarged ovaries and cysts and impacts fertility. Insulin-resistance is one of the main problems that women with PCOS have. The pancreas secretes too much insulin, causing inflammation, excess weight, impaired or irregular ovulation, and increased risk for type 2 diabetes and heart disease. Because berberine is effective in lowering blood sugar levels and helps with cholesterol, it is a compelling treatment option for women with PCOS.
Inflammation
One of the reasons berberine is so effective in treating cardiovascular and metabolic diseases is because of its antioxidant and anti-inflammatory properties.11 Berberine works at the molecular level to stabilize the oxidative stress in your body. Antioxidants like berberine protect your cells against free radicals, which are molecules produced when your body breaks down food or when you’re exposed to harmful chemicals like smoke or radiation. Some antioxidants are found naturally in the foods you eat – broccoli, spinach, carrots, avocados, sweet potatoes, and kale are a few examples. Berberine is a natural antioxidant supplement that works to inhibit oxidative stress in the liver, kidneys, and pancreas.
The anti-inflammatory activities of berberine happen at the cellular level and work through multiple, complex cellular kinases and signaling pathways. (For the cell biology gurus, these pathways include AMPK, mitogen-activated protein kinases (MAPKs), nuclear factor erythroid-2-related factor-2 (Nrf2) pathway, and the nuclear factor-κB (NF-κB) pathway.¹¹)
Bacterial Infection
Streptococcus agalactiae, or Group B Streptococcus (GBS), is a bacteria that can cause different kinds of serious infections, including pneumonia, sepsis, and meningitis. Berberine can enhance the effectiveness of antibiotics to treat GBS and other microbial bacterial infections, including MRSA.¹⁰
Canker Sores
Berberine can be produced in gel form. When applied as a gel to a canker sore on the mouth, it reduces the pain, redness, oozing, and size of the ulcer.⁶
Other Conditions
There is very promising but somewhat limited research on the positive effects of berberine in treating all of these conditions, too⁶:
- Burns
- Diarrhea that results from cholera or E. coli
- Non-cancerous growth in the large intestine and rectum (colorectal adenoma)
- Congestive Heart Failure (CHF)
- Heart Disease
- Swelling of the liver caused by Hepatitis B
- Irritable Bowel Syndrome (IBS)
- Low levels platelets in the blood (thrombocytopenia)
- Eye infection caused by Chlamydia trachomatis (trachoma)
- Tissue scarring caused by radiation therapy
- Glaucoma
- And more –
- https://shawnwells.com/2021/09/08/shawn-wells-on-berberine/
- https://shawnwells.com/2021/08/06/7-powerful-uses-of-berberine/
Dihydroberberine is berberine’s more biologically available derivative.
That means it’s the purer version of berberine. Berberine occasionally gets a bad rep because most of the berberine products available are not pure berberine. In fact, I’ve personally worked with 40 different berberine supplements in the laboratory and less than 10% of them were pure berberine (just 3 to be exact).12 Many companies that make these supplements add other ingredients or underdose the berberine. So, you have to use more of it to get the same effect. Using more of it leads to gastrointestinal discomfort, and a much higher price tag.
Dihydroberberine (DHB), on the other hand, has great bioavailability. The chemical structure of DHB makes it easy for the intestine to absorb when ingested. (Goodbye tummy troubles!) It is then oxidized back into berberine and sent into the plasma.¹² And, voila: DHB has the same powerful healing potential as berberine, but is needed in much smaller quantities and has fewer side effects. Research shows DHB has an intestinal absorption rate 5 times that of berberine!¹³ Just like berberine, DHB works to lower blood sugar and combat insulin sensitivity. Without a doubt, it is my top recommendation for anti-aging.
I recommend starting with 150 mg of DHB taken twice daily (e.g., morning and evening). DHB is longer lasting than berberine – it lasts for 8 hours instead of 4 hours. GlucoVantage is the patented berberine derivative that I suggest.
When you take DHB, you will see improved:
- Insulin insensitivity and carbohydrate tolerance
- Body composition (via AMPK, which drives carbs to the muscles rather than fats)
- Anti-aging (by reducing the glycation end-products that are associated with aging)
Potential Side Effects & Precautions
You should always be aware of potential side effects of any food, drink, medicine, or supplement you consume. The same is true for berberine (and DHB, for that matter). While berberine is considered safe for most adults, it’s not right for everyone. Side effects can include gastrointestinal issues like diarrhea, constipation, bloating, gas, and an upset stomach.6 Headaches may also be a side effect.
There are some cases where berberine should be taken with special precautions or not at all. These instances are:
Low Blood Pressure
Because berberine can lower blood pressure, it is typically not recommended for people who already have low pressure. Taking berberine may cause your blood pressure to drop too low. If you do use it, proceed with caution and under the care of a physician.⁶
Low Blood Sugar
Berberine is known to lower blood sugar. While it has shown to be as effective as pharmaceuticals like metformin and can be an important part of a treatment plan for some people with diabetes, it has the potential to lower blood sugar too much for some diabetics who already have low blood sugar if not properly managed. If you have diabetes and want to use berberine, be sure to work with your medical team.⁶
Pregnant or Breastfeeding
Do not take berberine if you are pregnant, planning to become pregnant, or breastfeeding. Berberine is considered unsafe for this population because it may cross the placenta and cause brain damage in the developing baby.⁶ Berberine may also be transferred through breast milk and cause harm to nursing babies.
Ask Coach Debbie abou t her personalized Coaching packages using her THE WHOLESTIC METHOD approach!
t her personalized Coaching packages using her THE WHOLESTIC METHOD approach!
Let’s work together to put your missing pieces of your health puzzle back together again so you can thrive as you age and live your best life in your second half of your life!
Improving metabolism and promoting weight loss in individuals with specific genetic predispositions (e.g., IRS1 and FTO SNPs), alongside hormonal imbalances (low thyroid, low cortisol, low estrogen, and high insulin), involves a multifaceted approach. This approach should be tailored to address genetic, hormonal, and lifestyle factors.
For example, here’s a comprehensive strategy:
1. Genetic Considerations
IRS1 and FTO SNPs:
- IRS1 SNPs: These can lead to insulin resistance and affect glucose metabolism.
- FTO SNPs: Associated with higher body mass index (BMI) and increased appetite.
2. Hormonal Balances
Thyroid (Hypothyroidism):
- Medications: Thyroid hormone replacement therapy (e.g., levothyroxine) as prescribed by your healthcare provider.
- Diet: Include iodine-rich foods (e.g., seaweed, fish), selenium (e.g., Brazil nuts), and zinc (e.g., pumpkin seeds) to support thyroid function.
- Exercise: Regular physical activity to boost metabolism.
Cortisol (Low Levels):
- Adaptogens: Herbal supplements like ashwagandha and rhodiola can help support adrenal function.
- Stress Management: Incorporate stress-reducing activities like yoga, meditation, and adequate sleep.
Estrogen (Low Levels):
- Phytoestrogens: Incorporate foods rich in phytoestrogens (e.g., soy, flaxseeds) to naturally support estrogen levels.
- Hormone Replacement Therapy: Consult your healthcare provider for potential estrogen therapy.
Insulin (High Levels/Insulin Resistance):
- Diet: Follow a low-glycemic index diet to manage blood sugar levels. Include fiber-rich foods, lean proteins, and healthy fats.
- Exercise: Regular cardiovascular and resistance training exercises to improve insulin sensitivity.
- Medications: In some cases, medications like metformin may be prescribed to improve insulin sensitivity.
3. Nutritional Strategy
- Balanced Diet: Focus on a diet that includes lean proteins, healthy fats, complex carbohydrates, and plenty of vegetables and fruits.
- Caloric Intake: Ensure you’re consuming an appropriate number of calories for weight loss, avoiding both excessive restriction and overeating.
- Meal Timing: Consider smaller, more frequent meals to stabilize blood sugar levels.
4. Lifestyle Modifications
- Regular Physical Activity: Aim for at least 150 minutes of moderate-intensity aerobic activity or 75 minutes of vigorous activity per week, along with muscle-strengthening activities on two or more days per week.
- Sleep Hygiene: Ensure 7-9 hours of quality sleep per night to support hormonal balance and weight management.
- Stress Reduction: Incorporate activities that reduce stress, such as mindfulness, meditation, or hobbies.
5. Monitoring and Adjustment
- Regular Check-ups: Frequent monitoring of thyroid levels, cortisol, estrogen, and insulin through blood tests.
- Professional Guidance: Work with a healthcare provider, endocrinologist, or a registered dietitian to adjust medications, supplements, and diet as needed.
6. Supplements (Consult with a Healthcare Provider Before Starting)
- Omega-3 Fatty Acids: Anti-inflammatory properties that support metabolic health.
- Probiotics: For gut health, which can influence metabolism and weight.
- Chromium: May improve insulin sensitivity and help with blood sugar control.
- Vitamin D: Supports overall health and can aid in weight management.
Improving metabolism and achieving weight loss with genetic and hormonal challenges requires a comprehensive and personalized approach. By addressing genetic predispositions, correcting hormonal imbalances, adopting a balanced diet, engaging in regular physical activity, and managing stress, you can effectively improve your metabolic health and facilitate weight loss. Regular monitoring and professional guidance are crucial to ensure the effectiveness and safety of your strategy.
but remember… you can’t out supplement poor lifestyle habits and you can’t out exercise a poor diet!









 t her personalized Coaching packages using her THE WHOLESTIC METHOD approach!
t her personalized Coaching packages using her THE WHOLESTIC METHOD approach!