Are you struggling to do all the right things and get the desired results?
results?
What is your Heart Rate Variability telling you about any signs and symptoms of HIDDEN sources of internal chronic stress plus stacked with chronic external sources of chronic stressors??
Hmmm….Here we go down another RABBIT HOLE: HRV & Gut Health
Heart Rate Variability (HRV) is a measure of the variation in time between each heartbeat, which is regulated by the autonomic nervous system (ANS). The ANS consists of two branches: the sympathetic nervous system (responsible for the “fight or flight” response) and the parasympathetic nervous system (responsible for the “rest and digest” response). HRV reflects the balance between these two branches.
Gut health, particularly conditions like leaky gut and chronic inflammation, can impact HRV through several mechanisms:
- Autonomic Nervous System Dysfunction: The gut has its own nervous system, known as the enteric nervous system (ENS), often called the “second brain.” It communicates bidirectionally with the central nervous system, influencing ANS function. Conditions like leaky gut and chronic inflammation can disrupt this communication, leading to dysregulation of the ANS and consequently affecting HRV.
- Inflammation: Chronic inflammation, which is often associated with gut health issues like leaky gut, can directly impact the autonomic nervous system and alter HRV. Inflammatory markers can affect the function of the vagus nerve, a key regulator of the parasympathetic branch of the ANS, thus affecting HRV.
- Microbiome: The gut microbiome plays a crucial role in regulating inflammation and immune responses throughout the body. Imbalances in the gut microbiota, such as dysbiosis (an imbalance between beneficial and harmful bacteria), can lead to chronic inflammation and affect ANS function, thereby influencing HRV.
- Stress Response: Gut health issues can cause stress on the body, activating the sympathetic nervous system and shifting the balance between sympathetic and parasympathetic activity. This alteration in autonomic balance can be reflected in changes in HRV.
- Vagus Nerve: The vagus nerve, which runs from the brainstem to the abdomen, plays a significant role in regulating both gut function and HRV. Dysfunction in the vagus nerve, often associated with conditions like leaky gut and chronic inflammation, can lead to alterations in HRV.
In summary, there is a complex interplay between gut health, including conditions like leaky gut and chronic inflammation, and HRV. Dysregulation in the gut can impact the autonomic nervous system, inflammation levels, stress response, and the gut-brain axis, all of which can manifest as changes in HRV. However, while there is evidence suggesting a connection between these factors, further research is needed to fully understand the extent and nuances of their relationship.
Is there a connection between your HRV and microbiome?
- The gut microbiome, comprising trillions of bacteria in the intestines, influences overall health, including digestion, immune function, and mental health.
- Gut microbiota regulate the immune system, produce nutrients, and maintain the intestinal barrier.
- The gut and heart communicate through the gut-brain axis involving the nervous, immune, and hormonal systems.
- Changes in the gut microbiome may affect heart rate variability (HRV), an indicator of autonomic nervous system function.
- Lower HRV is associated with gut dysbiosis, an imbalance in the gut microbiome.
- Interventions improving gut health, like probiotics or dietary changes, may enhance HRV.
- Disorders like irritable bowel syndrome and inflammatory bowel disease can disrupt HRV.
- Mice studies showed reduced HRV with disrupted microbiota and improved HRV with increased microbiota diversity through probiotics.
- Obesity is linked with decreased HRV, potentially connecting gut and heart health.
- Balanced microbiota are crucial for regulating various bodily functions, including HRV.
- Fiber-rich diets promote gut health.
- Certain gut microbial metabolites modulate the autonomic nervous system, potentially affecting HRV.
- Gut microbiota produce bioactive compounds like short-chain fatty acids, which may influence cardiovascular function.
- Research on the link between HRV and gut microbiota is still in its early stages.
- Understanding the gut-heart crosstalk may provide insights into human health and disease.
https://www.researchgate.net/publication/378680146_Heart_rate_variability_as_marker_of_gut_health
Does a LEAKY GUT impact your Heart Rate Variability?
Research on the direct impact of leaky gut on heart rate variability (HRV) is relatively limited compared to the broader research on gut health and HRV. However, there is growing interest in understanding the potential connection between leaky gut and alterations in autonomic nervous system (ANS) function, which could manifest as changes in HRV. Here’s an overview of the current understanding:
- The Gut-Heart Axis: The gut is intricately connected to the cardiovascular system through various pathways, including the autonomic nervous system, immune system, and inflammatory responses. Leaky gut, also known as increased intestinal permeability, refers to a condition where the intestinal barrier becomes compromised, allowing the passage of harmful substances like bacteria, toxins, and undigested food particles into the bloodstream.
- Inflammation and ANS Dysfunction: Leaky gut can trigger systemic inflammation and immune responses, which can affect ANS function. Chronic inflammation is associated with dysregulation of the sympathetic and parasympathetic branches of the ANS, leading to alterations in HRV. However, direct evidence linking leaky gut-induced inflammation to changes in HRV is still emerging.
- Vagus Nerve Dysfunction: The vagus nerve, a key component of the parasympathetic nervous system, plays a crucial role in regulating HRV. Dysfunction of the vagus nerve, which can occur due to inflammatory processes associated with leaky gut, may contribute to alterations in HRV.
- Clinical Studies: Some clinical studies have suggested an association between gastrointestinal conditions linked to leaky gut, such as irritable bowel syndrome (IBS) and inflammatory bowel disease (IBD), and changes in HRV. For example, individuals with IBS have been found to exhibit reduced HRV compared to healthy controls in some studies. However, more research is needed to establish a direct causal relationship between leaky gut and HRV alterations.
- Interventions and Observational Studies: Interventions aimed at improving gut health, such as probiotics, prebiotics, and dietary modifications, have shown promise in positively impacting HRV in some studies. These interventions may help restore gut barrier function and reduce inflammation, potentially leading to improvements in ANS function and HRV.
In summary, while there is growing interest in understanding the potential link between leaky gut and HRV, research in this area is still evolving. Further studies, including well-designed clinical trials and mechanistic investigations, are needed to elucidate the precise mechanisms underlying the relationship between gut health, leaky gut, and HRV.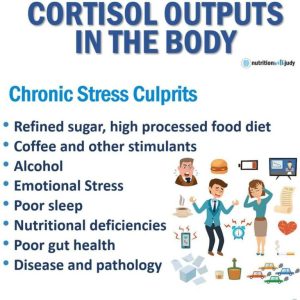
Leaky Gut and Chronic Inflammation on HRV
- The gut microbiome, vital for overall health, influences digestion, immune function, and mental health, regulating the immune system, producing nutrients, and maintaining the intestinal barrier.
- The gut and heart communicate through the gut-brain axis, involving the nervous, immune, and hormonal systems.
- Changes in the gut microbiome may impact heart rate variability (HRV), indicating autonomic nervous system function controlling heart rate and digestion.
- Lower HRV suggests less flexible autonomic function and is associated with gut dysbiosis.
- Interventions improving gut health, like probiotics or dietary changes, may enhance HRV.
- Disorders such as irritable bowel syndrome or inflammatory bowel disease can disrupt HRV.
- Mice studies show reduced HRV with a disrupted microbiota and improved HRV with increased microbiota diversity through probiotics.
- Obesity is linked with decreased HRV, potentially connecting gut and heart health.
- A balanced microbiota is essential for regulating various bodily functions, including HRV, with a fiber-rich diet being beneficial.
- Gut microbial metabolites and bioactive compounds, like short-chain fatty acids, may influence HRV and cardiovascular function.
- Research on HRV and gut microbiota is in early stages; mechanisms remain to be elucidated.
- Understanding gut-heart crosstalk offers avenues for further exploration and insights into human health and disease.
- https://www.researchgate.net/publication/378680146_Heart_rate_variability_as_marker_of_gut_health
Chronic Inflammation & HRV
Research on the relationship between chronic inflammation and heart rate variability (HRV) has uncovered several important findings:
- Inflammatory Markers and HRV: Studies have demonstrated that increased levels of inflammatory markers, such as C-reactive protein (CRP), interleukin-6 (IL-6), and tumor necrosis factor-alpha (TNF-alpha), are associated with reduced HRV. Chronic inflammation appears to negatively impact the autonomic nervous system, leading to decreased HRV.
- Disease Associations: Conditions characterized by chronic inflammation, such as rheumatoid arthritis, systemic lupus erythematosus (SLE), inflammatory bowel disease (IBD), and obesity, have been linked to alterations in HRV. These associations suggest that chronic inflammation may contribute to dysregulation of autonomic function, as reflected by changes in HRV.
- Cardiovascular Risk: Reduced HRV is considered a marker of increased cardiovascular risk. Chronic inflammation, by promoting endothelial dysfunction, atherosclerosis, and plaque instability, may contribute to cardiovascular disease development and progression, potentially mediated in part through alterations in HRV.
- Intervention Studies: Some research has explored the effects of anti-inflammatory interventions on HRV. For example, studies have investigated the impact of treatments such as statins, nonsteroidal anti-inflammatory drugs (NSAIDs), and anti-cytokine therapies on HRV parameters. While results have been mixed, some evidence suggests that reducing inflammation may improve HRV.
- Mechanistic Insights: Experimental studies in animal models and cell cultures have provided mechanistic insights into how inflammation affects autonomic function and HRV. Inflammatory cytokines can directly influence the activity of autonomic neurons and alter the balance between sympathetic and parasympathetic nervous system activity, thereby impacting HRV.
Overall, research indicates a complex interplay between chronic inflammation and HRV, with inflammation contributing to autonomic dysfunction and reduced HRV, which in turn may increase cardiovascular risk. Further studies are needed to elucidate the precise mechanisms underlying this relationship and to explore the potential therapeutic implications for managing cardiovascular health in individuals with chronic inflammatory conditions.
Solutions to improve your HRV: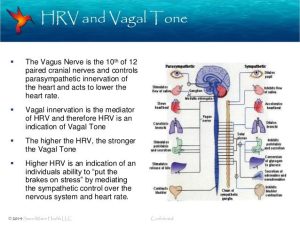
Here’s a list of strategies to improve heart rate variability (HRV), along with explanations of their mechanisms of action:
- Regular Physical Activity: Engaging in regular aerobic exercise, such as brisk walking, jogging, cycling, or swimming, can improve HRV. Exercise enhances autonomic nervous system function, increases parasympathetic activity, and reduces sympathetic dominance, leading to improved HRV.
- Stress Reduction Techniques: Stress reduction techniques such as mindfulness meditation, deep breathing exercises, yoga, and progressive muscle relaxation can help improve HRV by activating the parasympathetic nervous system and reducing sympathetic activation.
- Healthy Diet: Consuming a balanced diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats can support cardiovascular health and improve HRV. Certain nutrients, such as omega-3 fatty acids found in fish, have been associated with increased HRV.
- Adequate Sleep: Getting sufficient high-quality sleep is essential for optimal HRV. Sleep deprivation and poor sleep quality can disrupt autonomic nervous system function and decrease HRV. Aim for 7-9 hours of sleep per night in a comfortable sleep environment.
- Limiting Alcohol and Caffeine: Excessive alcohol consumption and high intake of caffeine can negatively impact HRV. Alcohol disrupts autonomic function, while caffeine can increase sympathetic activity. Limiting alcohol and caffeine intake, particularly close to bedtime, can help improve HRV.
- Smoking Cessation: Smoking is associated with reduced HRV due to its effects on the cardiovascular system and autonomic function. Quitting smoking can lead to improvements in HRV and overall cardiovascular health.
- Maintaining Hydration: Staying adequately hydrated is important for cardiovascular health and optimal autonomic function. Dehydration can lead to changes in blood volume and electrolyte balance, affecting HRV. Aim to drink plenty of water throughout the day.
- Mindful Breathing: Practicing slow, deep, diaphragmatic breathing can stimulate the vagus nerve, promoting parasympathetic activation and increasing HRV. Techniques such as coherent breathing, paced breathing, and resonance frequency breathing are effective for improving HRV.
- Biofeedback Therapy: Biofeedback training involves using electronic monitoring devices to provide real-time feedback on physiological parameters such as HRV. By learning to control their physiological responses, individuals can improve HRV and reduce stress.
- Supplementation: Some supplements, such as omega-3 fatty acids, magnesium, and adaptogenic herbs like ashwagandha and rhodiola rosea, have been suggested to support autonomic function and improve HRV. However, it’s important to consult with a healthcare professional before starting any supplementation regimen.
Implementing these strategies in combination can lead to significant improvements in HRV over time. It’s essential to adopt a holistic approach to cardiovascular health, incorporating lifestyle modifications, stress management techniques, and, if necessary, medical interventions under the guidance of a healthcare provider.
Here are some specific methods to improve heart rate variability (HRV):
- Deep Breathing Exercises: Engage in deep breathing exercises such as diaphragmatic breathing, also known as belly breathing. Inhale deeply through your nose, expanding your abdomen, and then exhale slowly through your mouth. Aim for a breathing rate of around 6 breaths per minute for optimal HRV improvement.
- Coherent Breathing: Practice coherent breathing, which involves breathing at a rhythm of 5 to 6 breaths per minute, with equal duration for inhalation and exhalation. This rhythmic breathing pattern can synchronize heart rate variability and promote relaxation.
- Mindfulness Meditation: Incorporate mindfulness meditation into your daily routine. Mindfulness practices focus on being present in the moment, observing thoughts and sensations without judgment. Regular meditation has been shown to increase HRV by reducing stress and promoting parasympathetic activity.
- Heart Rate Variability Biofeedback: Use biofeedback devices or smartphone apps that provide real-time feedback on HRV. By visualizing changes in HRV and learning to modulate their breathing and relaxation responses, individuals can improve HRV through biofeedback training.
- Progressive Muscle Relaxation: Practice progressive muscle relaxation, a technique that involves systematically tensing and relaxing different muscle groups in the body. This method promotes physical relaxation and reduces stress, leading to improvements in HRV.
- Yoga and Tai Chi: Participate in yoga or tai chi classes, which incorporate breath control, gentle movements, and mindfulness practices. These mind-body exercises have been shown to enhance HRV by reducing sympathetic nervous system activity and promoting relaxation.

- Cold Exposure: Incorporate cold exposure techniques such as cold showers or immersions in cold water. Cold exposure activates the sympathetic nervous system acutely but can lead to increased parasympathetic activity and improved HRV over time as the body adapts to the stressor.
- Aerobic Exercise: Engage in regular aerobic exercise such as walking, running, cycling, or swimming. Aerobic exercise improves cardiovascular fitness, enhances autonomic function, and increases HRV.
- Sleep Hygiene: Maintain good sleep hygiene habits to ensure restorative sleep. Establish a regular sleep schedule, create a comfortable sleep environment, limit exposure to electronic devices before bedtime, and practice relaxation techniques to promote deep sleep and improve HRV.
- Hydration and Nutrition: Stay hydrated by drinking an adequate amount of water throughout the day. Consume a balanced diet rich in whole foods, fruits, vegetables, lean proteins, and healthy fats to support overall health and improve HRV.
These specific methods can be integrated into your daily routine to promote heart rate variability and enhance overall well-being. It’s essential to experiment with different techniques and find what works best for you. Additionally, consistency and persistence are key to seeing long-term improvements in HRV.

