Are you fit and healthy from the inside out?
Research on the correlation between leaky gut and endurance exercise in athletes is an evolving field, with some studies suggesting a potential link between intense exercise, gut permeability, and gastrointestinal symptoms.
- Fatigue, mood disturbances, under performance and gastrointestinal distress are common among athletes during training and competition. The psychosocial and physical demands during intense exercise can initiate a stress response activating the sympathetic-adrenomedullary and hypothalamus-pituitary-adrenal (HPA) axes, resulting in the release of stress and catabolic hormones, inflammatory cytokines and microbial molecules.
- The gut is home to trillions of microorganisms that have fundamental roles in many aspects of human biology, including metabolism, endocrine, neuronal and immune function.
- The gut microbiome and its influence on host behavior, intestinal barrier and immune function are believed to be a critical aspect of the brain-gut axis.
- Recent evidence in murine models shows that there is a high correlation between physical and emotional stress during exercise and changes in gastrointestinal microbiota composition.
- For instance, induced exercise-stress decreased cecal levels of Turicibacter spp and increased Ruminococcus gnavus, which have well defined roles in intestinal mucus degradation and immune function.
- Diet is known to dramatically modulate the composition of the gut microbiota.
- Due to the considerable complexity of stress responses in elite athletes (from leaky gut to increased catabolism and depression), defining standard diet regimes is difficult.
- However, some preliminary experimental data obtained from studies using probiotics and prebiotics studies show some interesting results, indicating that the microbiota acts like an endocrine organ (e.g. secreting serotonin, dopamine or other neurotransmitters) and may control the HPA axis in athletes.
- What is troubling is that dietary recommendations for elite athletes are primarily based on a low consumption of plant polysaccharides, which is associated with reduced microbiota diversity and functionality (e.g. less synthesis of byproducts such as short chain fatty acids and neurotransmitters).
- As more elite athletes suffer from psychological and gastrointestinal conditions that can be linked to the gut, targeting the microbiota therapeutically may need to be incorporated in athletes’ diets that take into consideration dietary fiber as well as microbial taxa not currently present in athlete’s gut.
- Exercise-induced stress behavior, gut-microbiota-brain axis and diet: a systematic review for athletes

All disease begins in the (leaky) gut: role of zonulin-mediated gut permeability in the pathogenesis of some chronic inflammatory diseases
Abstract
Improved hygiene leading to reduced exposure to microorganisms has been implicated as one possible cause for the recent “epidemic” of chronic inflammatory diseases (CIDs) in industrialized countries. That is the essence of the hygiene hypothesis that argues that rising incidence of CIDs may be, at least in part, the result of lifestyle and environmental changes that have made us too “clean” for our own good, so causing changes in our microbiota. Apart from genetic makeup and exposure to environmental triggers, inappropriate increase in intestinal permeability (which may be influenced by the composition of the gut microbiota), a “hyper-belligerent” immune system responsible for the tolerance–immune response balance, and the composition of gut microbiome and its epigenetic influence on the host genomic expression have been identified as three additional elements in causing CIDs. During the past decade, a growing number of publications have focused on human genetics, the gut microbiome, and proteomics, suggesting that loss of mucosal barrier function, particularly in the gastrointestinal tract, may substantially affect antigen trafficking, ultimately influencing the close bidirectional interaction between gut microbiome and our immune system. This cross-talk is highly influential in shaping the host gut immune system function and ultimately shifting genetic predisposition to clinical outcome. This observation led to a re-visitation of the possible causes of CIDs epidemics, suggesting a key pathogenic role of gut permeability. Pre-clinical and clinical studies have shown that the zonulin family, a group of proteins modulating gut permeability, is implicated in a variety of CIDs, including autoimmune, infective, metabolic, and tumoral diseases. These data offer novel therapeutic targets for a variety of CIDs in which the zonulin pathway is implicated in their pathogenesis.
Keywords: Chronic inflammatory diseases, Gut permeability, microbiome, zonulin
https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6996528/
Here are some key findings from relevant research:
- Increased Intestinal Permeability: Endurance exercise, particularly prolonged and intense bouts, has been associated with increased intestinal permeability, commonly referred to as “leaky gut.” This increased permeability allows for the passage of larger molecules (such as bacteria, toxins, and undigested food particles) through the intestinal barrier, potentially triggering immune responses and inflammation.
- Gastrointestinal Symptoms in Athletes: Endurance athletes, such as marathon runners, triathletes, and cyclists, frequently report gastrointestinal symptoms during or after exercise, including bloating, abdominal pain, diarrhea, and nausea. These symptoms may be indicative of gut dysfunction or increased permeability.
- Mechanisms of Gut Permeability: Several mechanisms have been proposed to explain the relationship between endurance exercise and gut permeability. These include decreased blood flow to the gut during intense exercise, oxidative stress, release of inflammatory cytokines, alterations in gut microbiota composition, and changes in intestinal tight junction proteins that regulate barrier function.
- Impact on Performance and Recovery: The presence of leaky gut and gastrointestinal symptoms in athletes may impair performance, hinder recovery, and increase susceptibility to infections and inflammatory conditions. Chronic exposure to exercise-induced gut stress could also contribute to long-term health consequences, although more research is needed to fully understand these effects.
- Nutritional Strategies: Nutritional interventions, such as dietary modification, supplementation with probiotics or specific nutrients (e.g., glutamine, zinc), and timing of food intake, may help mitigate exercise-induced gut damage and improve gut health in athletes. However, the efficacy of these strategies remains to be fully elucidated.
Overall, while there is growing evidence suggesting a correlation between endurance exercise, gut permeability, and gastrointestinal symptoms in athletes, further research is needed to better understand the underlying mechanisms and develop targeted interventions to optimize gut health and performance in this population.
Abstract
The microorganisms in the gastrointestinal tract play a significant role in nutrient uptake, vitamin synthesis, energy harvest, inflammatory modulation, and host immune response, collectively contributing to human health.
Important factors such as age, birth method, antibiotic use, and diet have been established as formative factors that shape the gut microbiota.
- Yet, less described is the role that exercise plays, particularly how associated factors and stressors, such as sport/exercise-specific diet, environment, and their interactions, may influence the gut microbiota.
- In particular, high-level athletes offer remarkable physiology and metabolism (including muscular strength/power, aerobic capacity, energy expenditure, and heat production) compared to sedentary individuals, and provide unique insight in gut microbiota research.
- In addition, the gut microbiota with its ability to harvest energy, modulate the immune system, and influence gastrointestinal health, likely plays an important role in athlete health, wellbeing, and sports performance.
- Therefore, understanding the mechanisms in which the gut microbiota could play in the role of influencing athletic performance is of considerable interest to athletes who work to improve their results in competition as well as reduce recovery time during training. Ultimately this research is expected to extend beyond athletics as understanding optimal fitness has applications for overall health and wellness in larger communities.
- Therefore, the purpose of this narrative review is to summarize current knowledge of the athletic gut microbiota and the factors that shape it.
- Exercise, associated dietary factors, and the athletic classification promote a more “health-associated” gut microbiota.
- Such features include a higher abundance of health-promoting bacterial species, increased microbial diversity, functional metabolic capacity, and microbial-associated metabolites, stimulation of bacterial abundance that can modulate mucosal immunity, and improved gastrointestinal barrier function.
https://www.tandfonline.com/doi/full/10.1186/s12970-020-00353-w
The correlation between leaky gut and exercise is multifactorial and involves various physiological mechanisms.
Abstract
- The intestinal barrier is complex and consists of multiple layers, and it provides a physical and functional barrier to the transport of luminal contents to systemic circulation.
- While the epithelial cell layer and the outer/inner mucin layer constitute the physical barrier and are often referred to as the intestinal barrier, intestinal alkaline phosphatase (IAP) produced by epithelial cells and antibacterial proteins secreted by Panneth cells represent the functional barrier.
- While antibacterial proteins play an important role in the host defense against gut microbes, IAP detoxifies bacterial endotoxin lipopolysaccharide (LPS) by catalyzing the dephosphorylation of the active/toxic Lipid A moiety, preventing local inflammation as well as the translocation of active LPS into systemic circulation.
- The causal relationship between circulating LPS levels and the development of multiple diseases underscores the importance of detailed examination of changes in the “layers” of the intestinal barrier associated with disease development and how this dysfunction can be attenuated by targeted interventions.
- To develop targeted therapies for improving intestinal barrier function, it is imperative to have a deeper understanding of the intestinal barrier itself, the mechanisms underlying the development of diseases due to barrier dysfunction (eg, high circulating LPS levels), the assessment of intestinal barrier function under diseased conditions, and of how individual layers of the intestinal barrier can be beneficially modulated to potentially attenuate the development of associated diseases.
- This review summarizes the current knowledge of the composition of the intestinal barrier and its assessment and modulation for the development of potential therapies for barrier dysfunction-associated diseases.
- https://academic.oup.com/jes/article/4/2/bvz039/5741771
Summary and Conclusions
- The causal relationship between chronic inflammation and the development of multiple diseases is increasingly being established, and the likely trigger for this low level, yet sustained systemic inflammation, is bacterial endotoxin LPS.
- While dietary components or intestinal injury (eg, by ischemia/reperfusion) may initiate the release of LPS from intestinal lumen to systemic circulation, the physical as well as the functional integrity of the intestinal barrier is the critical determinant of this translocation.
- This review summarizes the composition of the intestinal barrier, consequences of a dysfunctional barrier, and elaborates on the role of translocated LPS in the development of diseases.
- In addition, current knowledge on the successful manipulation of individual “layers” of the intestinal barrier is summarized.
- Discussion of the currently available tests emphasize the future use of the status of barrier function as a diagnostic parameter facilitating demonstration of causal relationship with pathogenesis of disease.
- The development of novel and more specific tests are expected to facilitate the identification of individual “layers” affected in a given disease process or person, leading to targeted interventions.
- For example, exogenous IAP supplementation or curcumin-mediated increase in IAP activity would be the therapeutic option where loss of IAP is identified.
- Galactooligosaccharide fiber supplementation would be the preferred option where mucosal layer disruption is evident. Phytochemicals and other nutritional supplements (eg, vitamin D) with demonstrated effects on improvement of tight junction protein expression/function are likely to be most beneficial where these disruptions are noted.
- Therefore, while correcting intestinal barrier dysfunction for modulation of multiple diseases can be envisioned as a viable therapeutic option, continuing progress in identifying the precise defect by use of specific biomarkers would facilitate targeted interventions.
What is metabolic endotoxemia? LPS?
Here are some reasons why exercise, particularly intense or prolonged endurance exercise, may contribute to increased intestinal permeability (leaky gut):
- Decreased Blood Flow to the Gut: During exercise, blood flow is redirected away from the gastrointestinal tract to the working muscles and other vital organs. This reduction in blood flow to the gut can compromise intestinal barrier function, leading to increased permeability.
- Oxidative Stress: Intense exercise generates reactive oxygen species (ROS) and oxidative stress within the body. Excessive ROS production can damage intestinal epithelial cells and disrupt tight junction proteins, which play a crucial role in maintaining the integrity of the intestinal barrier.
- Inflammatory Response: Endurance exercise can trigger an inflammatory response in the body, characterized by the release of pro-inflammatory cytokines. Chronic inflammation may contribute to alterations in gut permeability by disrupting tight junctions and increasing intestinal permeability.
- Gut Microbiota Changes: Exercise can influence the composition and diversity of the gut microbiota. Dysbiosis, or an imbalance in the gut microbiota, has been associated with increased intestinal permeability and gastrointestinal dysfunction. Changes in the gut microbiota induced by exercise may contribute to alterations in gut barrier function.
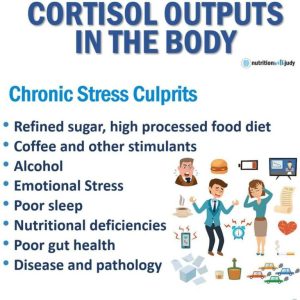
- Hormonal Changes: Exercise can lead to alterations in hormone levels, including increases in cortisol, adrenaline, and other stress hormones. These hormonal changes may affect gut motility, blood flow, and immune function, potentially compromising intestinal barrier integrity.
- Hydration and Nutritional Factors: Dehydration and inadequate nutrition during exercise may exacerbate gut permeability. Proper hydration and nutrition are essential for maintaining optimal gastrointestinal function and barrier integrity during exercise.
- Individual Variability: It’s important to recognize that not all individuals experience exercise-induced changes in gut permeability to the same extent. Factors such as genetics, training status, exercise intensity and duration, diet, and overall health status can influence individual susceptibility to exercise-induced gut dysfunction.
Overall, the correlation between leaky gut and exercise involves a complex interplay of physiological factors, and further research is needed to fully understand the mechanisms underlying this relationship. Despite the potential negative effects of exercise on gut permeability, regular physical activity has numerous health benefits and should be balanced with strategies to support gut health and recovery.
Dr. Fasano on Gut health:
Dr. Alessio Fasano is a renowned expert in the field of celiac disease and gluten-related disorders. His research has significantly contributed to our understanding of the mechanisms behind these conditions, including the concept of “leaky gut” and its potential role in chronic inflammatory diseases.
Some key findings and contributions from Dr. Fasano’s research include:
- Role of Zonulin: Dr. Fasano and his team discovered zonulin, a protein that regulates the tight junctions between cells in the intestinal lining. Elevated levels of zonulin have been associated with increased intestinal permeability, or “leaky gut,” which is implicated in various autoimmune and inflammatory conditions.
- Connection to Celiac Disease: Dr. Fasano’s research has significantly advanced our understanding of celiac disease, an autoimmune disorder triggered by the ingestion of gluten in genetically predisposed individuals. He has studied the mechanisms by which gluten activates the immune response and damages the intestinal lining in celiac disease.
- Non-Celiac Gluten Sensitivity (NCGS): Dr. Fasano has also investigated non-celiac gluten sensitivity, a condition characterized by symptoms similar to those of celiac disease but without the autoimmune response or intestinal damage seen in celiac disease. His research has helped elucidate the mechanisms underlying NCGS and differentiate it from celiac disease.
- Association with Chronic Inflammatory Diseases: Dr. Fasano’s work has explored the potential links between intestinal permeability, gluten, and chronic inflammatory diseases beyond celiac disease, including autoimmune conditions such as rheumatoid arthritis, multiple sclerosis, and inflammatory bowel disease (IBD). His research suggests that intestinal permeability may contribute to the development or exacerbation of these conditions by allowing the passage of harmful substances into the bloodstream.
Overall, Dr. Fasano’s research has shed light on the complex interactions between the gut, the immune system, and environmental factors such as gluten, leading to a better understanding of celiac disease, non-celiac gluten sensitivity, and their potential roles in chronic inflammatory diseases. His work has paved the way for further research and therapeutic strategies aimed at managing these conditions.
Dr. Alessio Fasano’s research on gut health, inflammation, and leaky gut has led to several suggestions for improving these conditions.
While individual recommendations may vary based on specific health needs, some general strategies suggested by his research include:
- Gluten-Free Diet: For individuals with celiac disease or non-celiac gluten sensitivity (NCGS), adopting a strict gluten-free diet is essential. Avoiding gluten-containing grains such as wheat, barley, and rye can help reduce inflammation, heal the intestinal lining, and alleviate symptoms associated with these conditions.
- Balanced Diet: Consuming a diverse range of whole, unprocessed foods is crucial for supporting gut health and reducing inflammation. Emphasize fruits, vegetables, lean proteins, healthy fats, and gluten-free grains to provide essential nutrients and promote a healthy balance of gut bacteria.
- Probiotics: Incorporating probiotic-rich foods or supplements into your diet can help restore and maintain a healthy balance of gut bacteria. Probiotics may support digestion, strengthen the gut barrier, and reduce inflammation. Fermented foods like yogurt, kefir, sauerkraut, kimchi, and kombucha are good natural sources of probiotics.
- Prebiotics: Including prebiotic-rich foods in your diet can help nourish beneficial gut bacteria and promote their growth. Prebiotics are non-digestible fibers found in foods like chicory root, Jerusalem artichokes, garlic, onions, leeks, asparagus, bananas, apples, flaxseeds, and oats.
- Omega-3 Fatty Acids: Omega-3 fatty acids, found in fatty fish (such as salmon, mackerel, and sardines), flaxseeds, chia seeds, and walnuts, have anti-inflammatory properties that can help reduce inflammation in the gut and throughout the body.
- Stress Management: Chronic stress can contribute to gut inflammation and compromise gut barrier function. Practicing stress-reducing techniques such as mindfulness, meditation, yoga, deep breathing exercises, and regular physical activity can help support gut health and reduce inflammation.
- Avoiding Gut Irritants: Limiting or avoiding substances that can irritate the gut lining, such as alcohol, caffeine, processed foods, artificial additives, and certain medications (like nonsteroidal anti-inflammatory drugs or NSAIDs), may help reduce inflammation and promote gut healing.
- Hydration: Drinking an adequate amount of water is essential for maintaining proper hydration and supporting healthy digestion and gut function. Aim to drink plenty of water throughout the day to stay hydrated.
What is GLIADIN ?
?
The part of wheat that impacts the gut wall lining tight junctions is primarily a protein called gliadin, which is found in gluten-containing grains such as wheat, barley, and rye.
Gliadin is a component of gluten, and it plays a key role in triggering immune responses in individuals with celiac disease and potentially contributing to gut permeability or “leaky gut” in some individuals without celiac disease.
Gliadin is a protein component found in gluten, a mixture of proteins found in wheat and related grains like barley and rye. It belongs to a group of proteins called prolamins. Gliadin is one of the main proteins responsible for the elastic texture of dough, which allows bread to rise and gives it its chewy texture.
In individuals with celiac disease, gliadin can trigger an immune response, leading to damage to the small intestine. This immune reaction is a key aspect of the autoimmune response seen in celiac disease, where the body’s immune system mistakenly attacks its own tissues in response to gluten ingestion. As a result, individuals with celiac disease must strictly avoid foods containing gliadin and other gluten-containing grains to prevent adverse health effects.
Gliadin levels can be increased through various means, primarily through the consumption of gluten-containing grains such as wheat, barley, and rye. These grains are common ingredients in many processed foods, bread, pasta, cereals, and baked goods. Therefore, a diet rich in these grains will naturally lead to higher gliadin intake.
The impact of gliadin on gut health is significant, particularly in individuals with conditions like celiac disease or non-celiac gluten sensitivity.
Here’s how gliadin affects gut health:
- Celiac Disease: In individuals with celiac disease, gliadin triggers an autoimmune response that damages the lining of the small intestine. This damage leads to villous atrophy, where the finger-like projections in the small intestine called villi become flattened, reducing the surface area available for nutrient absorption. This can lead to malabsorption of nutrients, resulting in various symptoms such as diarrhea, weight loss, fatigue, and nutritional deficiencies.
- Non-Celiac Gluten Sensitivity (NCGS): Some individuals experience gastrointestinal symptoms similar to those of celiac disease when they consume gluten-containing foods, but they do not test positive for celiac disease or wheat allergy. This condition is referred to as non-celiac gluten sensitivity. While the exact mechanisms are not fully understood, gliadin and other components of gluten are believed to play a role in triggering symptoms in these individuals.

- Leaky Gut: Gliadin has been implicated in increasing intestinal permeability, a condition often referred to as “leaky gut.” In individuals with increased intestinal permeability, the tight junctions between cells in the intestinal lining become compromised, allowing larger molecules, toxins, and pathogens to pass through the intestinal barrier and enter the bloodstream. This can trigger an immune response and inflammation in the body.
- Chronic Inflammation: Gliadin-induced intestinal damage and increased intestinal permeability can lead to chronic inflammation not only in the gut but also systemically throughout the body. Chronic inflammation is associated with various health conditions, including inflammatory bowel diseases (such as Crohn’s disease and ulcerative colitis), autoimmune disorders, metabolic syndrome, and cardiovascular diseases.
Overall, while gliadin is a normal component of gluten-containing grains and is harmless for most people, it can have significant adverse effects on gut health in susceptible individuals, particularly those with celiac disease or non-celiac gluten sensitivity. Moreover, its role in promoting leaky gut and chronic inflammation highlights its potential impact on overall health beyond the gut.
Here’s how gliadin affects tight junctions in the gut wall:
- Immune Response Activation: In individuals with celiac disease, the ingestion of gluten-containing foods leads to the activation of the immune system. Gliadin triggers an immune response in the small intestine, leading to inflammation and damage to the intestinal lining.
- Zonulin Release: Gliadin has been shown to increase the production of a protein called zonulin in the gut. Zonulin regulates the opening and closing of the tight junctions between intestinal epithelial cells, which control the permeability of the intestinal barrier.
- Tight Junction Disruption: Elevated levels of zonulin induced by gliadin can result in the loosening of tight junctions between epithelial cells in the intestinal lining. This increased permeability allows larger molecules, such as undigested proteins, toxins, and bacteria, to pass through the intestinal barrier and enter the bloodstream. This phenomenon is often referred to as “leaky gut.”
- Inflammation and Immune Activation: The passage of larger molecules through the compromised intestinal barrier can trigger an immune response and inflammation in the body. This immune activation may contribute to the development or exacerbation of various health conditions, including autoimmune diseases, allergic reactions, and chronic inflammation.
It’s important to note that while gliadin plays a significant role in triggering gut barrier dysfunction in individuals with celiac disease, non-celiac gluten sensitivity (NCGS), and potentially in some individuals without gluten-related disorders, the mechanisms involved may vary among individuals. Additionally, other components of wheat and gluten may also contribute to gut inflammation and permeability in susceptible individuals.
Improving the integrity of tight junctions in the gut wall is crucial for maintaining gut health and reducing the risk of conditions associated with increased intestinal permeability, such as leaky gut syndrome. Here are some strategies to help improve tight junction function:
- Dietary Changes:
- Avoid Inflammatory Foods: Limit or avoid foods that can contribute to inflammation in the gut, such as processed foods, refined sugars, excessive alcohol, and certain food additives.
- Emphasize Whole Foods: Focus on a diet rich in whole, nutrient-dense foods, including fruits, vegetables, lean proteins, healthy fats, and whole grains (for individuals who tolerate them).
- Consider Eliminating Trigger Foods: Some individuals may benefit from identifying and eliminating specific trigger foods that exacerbate gut symptoms, such as gluten-containing grains or dairy products.
- Include Gut-Supportive Nutrients: Consume foods rich in nutrients that support gut health, such as omega-3 fatty acids (found in fatty fish, flaxseeds, and walnuts), fiber (from fruits, vegetables, and whole grains), and antioxidants (found in colorful fruits and vegetables).
- Supplements:
- Probiotics: Certain probiotic strains, such as Lactobacillus and Bifidobacterium species, have been shown to support gut barrier function and improve tight junction integrity. Consider incorporating probiotic-rich foods like yogurt, kefir, sauerkraut, or taking a probiotic supplement.
- Glutamine: Glutamine is an amino acid that plays a role in maintaining the integrity of the intestinal mucosa and supporting tight junction function. It can be obtained through dietary sources like meat, fish, dairy, and legumes, or taken as a supplement.
- Quercetin: Quercetin is a flavonoid with anti-inflammatory and antioxidant properties that may help support gut barrier function. It is found in foods like onions, apples, berries, and green tea, or available in supplement form.
- Stress Management:
- Chronic stress can contribute to gut barrier dysfunction. Practice stress-reducing techniques such as mindfulness meditation, deep breathing exercises, yoga, or engaging in hobbies and activities that promote relaxation.
- Sleep Quality:
- Prioritize adequate sleep, as insufficient sleep or poor sleep quality can impair gut barrier function and contribute to inflammation. Aim for 7-9 hours of quality sleep per night.
- Exercise:
- Regular physical activity has been shown to have beneficial effects on gut health. Aim for a combination of aerobic exercise, strength training, and flexibility exercises for overall health and gut function.
- Avoid Gut Irritants:
- Minimize exposure to substances that can irritate the gut lining, such as nonsteroidal anti-inflammatory drugs (NSAIDs) and certain medications that may disrupt gut barrier function.
- Work with a Healthcare Provider:
- If you suspect you have gut health issues or if you’re considering significant dietary or lifestyle changes, it’s advisable to consult with a healthcare provider, such as a registered dietitian or gastroenterologist, who can provide personalized recommendations and monitor your progress. They may also conduct tests to assess gut health and identify any underlying conditions that need to be addressed.
Wheat grown in North America and Europe can differ in several aspects, including genetic composition, cultivation practices, and processing methods.
Here are some key differences:
- Genetic Composition: North American wheat varieties often belong to the hard red and soft red wheat classes, while Europe primarily cultivates hard wheat varieties like hard red and hard white wheat. The genetic differences between these varieties can influence factors such as protein content, gluten strength, and baking characteristics.
- Growing Conditions: Wheat cultivation practices may vary between North America and Europe due to differences in climate, soil conditions, and agricultural practices. For example, North American wheat-growing regions, such as the Great Plains in the United States and the Canadian Prairies, are known for their vast expanses of wheat fields and dryland farming practices. In contrast, European wheat cultivation may occur in diverse climates, including temperate regions with more moderate temperatures and higher rainfall.
- Pesticide Use: Regulations regarding pesticide use and genetically modified organisms (GMOs) differ between North America and Europe. While genetically modified wheat is not commercially grown in either region, there may be variations in pesticide usage and agricultural practices that impact wheat production and quality.
- Processing Methods: Wheat processing methods can vary between North America and Europe, affecting the characteristics of wheat-based products. For example, in Europe, traditional stone milling methods are still used in some regions, resulting in flour with different particle sizes and nutrient profiles compared to flour produced using modern roller milling techniques more common in North America.
- Food Additives and Labeling: There may be differences in food additives, preservatives, and labeling regulations between North America and Europe. For instance, European Union regulations on food additives and labeling requirements may differ from those in North America, impacting the ingredients and information provided on wheat-based products.
- Cultural Preferences: Cultural preferences and culinary traditions can influence the types of wheat products consumed in North America and Europe. For example, bread is a staple food in many European countries, and there is a rich tradition of artisanal breadmaking. In contrast, North American diets may include a wider variety of wheat-based products, including breakfast cereals, pastries, and pasta.
Overall, while wheat is a globally important crop, there are notable differences in its cultivation, processing, and consumption between North America and Europe, reflecting regional agricultural practices, preferences, and regulatory environments.
Repairing and re-sealing a damaged gut wall and mucosa, commonly associated with conditions like leaky gut syndrome, involves adopting a multifaceted approach that addresses underlying causes, supports gut healing, and promotes overall gut health.
Here are some strategies to consider in a restore and repair protocol…but work with a practitioner!
- Identify and Remove Triggering Factors: Identify and remove any factors that may be contributing to gut wall damage, such as dietary triggers (e.g., gluten, processed foods, food sensitivities), medications (e.g., nonsteroidal anti-inflammatory drugs or NSAIDs), infections, stress, and environmental toxins.
- Adopt a Gut-Friendly Diet:
- Focus on whole, unprocessed foods rich in fiber, vitamins, and minerals.
- Include plenty of fruits, vegetables, legumes, nuts, seeds, and gluten-free whole grains.
- Consider incorporating gut-healing foods such as bone broth, collagen peptides, fermented foods (e.g., sauerkraut, kimchi, kefir), and omega-3 fatty acids.
- Avoid or minimize consumption of inflammatory foods, including refined sugars, artificial additives, processed foods, and potential allergens or irritants.
- Support Digestive Enzymes: Consider incorporating digestive enzyme supplements to aid in the breakdown and absorption of nutrients, particularly if there are digestive issues or deficiencies present.
- Promote Gut Microbiome Health:
- Consume prebiotic-rich foods to nourish beneficial gut bacteria.
- Incorporate probiotic-rich foods or supplements to restore and maintain a healthy balance of gut flora.
- Consider synbiotic supplements that combine prebiotics and probiotics for synergistic effects.
- Manage Stress: Practice stress-reduction techniques such as mindfulness, meditation, deep breathing exercises, yoga, and regular physical activity to help mitigate the impact of stress on gut health.

Digestion & Gut Health - Heal with Nutrients and Supplements:
- Consider supplementing with gut-healing nutrients such as glutamine, zinc, vitamin D, omega-3 fatty acids, and certain herbs (e.g., slippery elm, marshmallow root, aloe vera).
- Consult with a healthcare professional or registered dietitian to determine appropriate dosages and formulations based on individual needs.
- Address Gut Dysbiosis and Infections: Work with a healthcare provider to identify and address any underlying gut dysbiosis (imbalance of gut bacteria) or infections that may be contributing to gut wall damage.
- Promote Mucosal Healing: Certain nutrients and compounds, such as butyrate (a short-chain fatty acid), quercetin, and glutathione, have been shown to support mucosal healing and repair. Incorporate foods rich in these nutrients or consider supplementation under the guidance of a healthcare provider.
- Stay Hydrated: Drink plenty of water to support hydration and mucous membrane function in the gut.
- Seek Professional Guidance: Consult with a healthcare provider, such as a gastroenterologist, functional medicine practitioner, or registered dietitian, who can provide personalized guidance and recommendations based on your specific health status, symptoms, and medical history.
It’s important to approach gut healing holistically and be patient, as it may take time to see improvements. Additionally, individual responses to interventions may vary, so it’s essential to listen to your body and work with qualified professionals to develop a comprehensive and sustainable gut-healing plan.
Tips to improve the good bacteria in our gut!
- Prebiotics:
- Definition: Prebiotics are non-digestible fibers that serve as food for the beneficial bacteria in your gut. They help stimulate the growth and activity of these bacteria.
- Purpose: Prebiotics support the growth of probiotics (beneficial bacteria) in the gut, which can improve gut health, enhance digestion, boost the immune system, and potentially reduce inflammation.
- Sources: Prebiotics are found in various plant-based foods, including:
- Chicory root
- Jerusalem artichokes
- Dandelion greens
- Garlic
- Onions
- Leeks
- Asparagus
- Bananas (especially slightly green ones)
- Apples
- Flaxseeds
- Postbiotics:
- Definition: Postbiotics are the byproducts or metabolites produced by probiotic bacteria during fermentation or other metabolic processes. These can include short-chain fatty acids, organic acids, peptides, and other bioactive compounds.
- Purpose: Postbiotics can have various health benefits, including supporting gut health, reducing inflammation, improving immune function, and potentially providing protection against pathogens.
- Sources: Postbiotics are naturally produced by probiotic bacteria during fermentation processes. Foods containing probiotics or fermented foods such as yogurt, kefir, sauerkraut, and kimchi can contain postbiotics.
- Synbiotics:

- Definition: Synbiotics are a combination of prebiotics and probiotics. They are designed to work synergistically, with the prebiotics providing food for the probiotics, thereby enhancing their survival and activity in the gut.
- Purpose: Synbiotics aim to improve the survival, implantation, and activity of probiotics in the gut, leading to enhanced health benefits such as improved digestion, immune function, and gut health.
- Sources: Synbiotics can be found in certain foods or supplements that contain both prebiotics and probiotics. For example, some yogurts may contain added prebiotics to support the probiotics naturally found in yogurt cultures.
- Probiotics:
- Definition: Probiotics are live microorganisms, primarily bacteria but also some yeasts, that provide health benefits when consumed in adequate amounts. They colonize the gut and contribute to the balance of the gut microbiota.
- Purpose: Probiotics help maintain a healthy balance of gut bacteria, support digestion, boost the immune system, and may have other health benefits such as reducing inflammation and improving mental health.
- Sources: Probiotics can be found in fermented foods and dietary supplements. Common food sources include yogurt, kefir, kimchi, sauerkraut, miso, tempeh, and kombucha. Probiotic supplements are also available in various forms such as capsules, tablets, powders, and liquids. When choosing probiotic supplements, look for products that contain well-researched strains and are manufactured by reputable brands.
By incorporating prebiotics, probiotics, postbiotics, and synbiotics into your diet, you can support a healthy gut microbiome, which in turn can have positive effects on overall health and well-being.
Fiber is essential for feeding the beneficial bacteria in your gut microbiome, but there are certain foods that can provide similar benefits if you’re looking for alternatives:
- Prebiotic Foods: These are rich in fibers that nourish beneficial bacteria in the gut. Examples include:
- Chicory root
- Jerusalem artichokes
- Dandelion greens
- Garlic
- Onions
- Leeks
- Asparagus
- Bananas (especially slightly green ones)
- Apples
- Flaxseeds
- Oats
- Resistant Starches: These are starches that resist digestion in the small intestine and reach the colon intact, where they can be fermented by gut bacteria. Foods high in resistant starch include:
- Green bananas
- Raw oats
- Cooked and cooled potatoes
- Legumes (beans, lentils, chickpeas)
- Whole grains (barley, rye)
- Cooked and cooled rice
- Firm bananas
- Polyphenol-Rich Foods: Polyphenols are compounds found in plant foods that have antioxidant properties and can influence the composition of gut bacteria. Examples include:
- Berries (blueberries, strawberries, raspberries)
- Apples
- Citrus fruits
- Red grapes
- Green tea
- Dark chocolate
- Nuts (particularly almonds)
- Fermented Foods: While not directly providing fiber, fermented foods contain probiotics which can support gut health by introducing beneficial bacteria. Examples include:
- Yogurt (with live and active cultures)

- Kefir
- Kimchi
- Sauerkraut
- Miso
- Tempeh
- Kombucha
- Yogurt (with live and active cultures)
Incorporating a variety of these foods into your diet can help promote a diverse and healthy gut microbiome, even if you’re not getting fiber from traditional sources like whole grains and vegetables. However, it’s still important to consume fiber-rich foods for overall health benefits. Or is it?
What about your vagal tone?
The vagus nerve, also known as the tenth cranial nerve, plays a crucial role in the communication between the gut and the brain. It forms part of the autonomic nervous system, which controls involuntary bodily functions such as heart rate, digestion, and respiratory rate. The vagus nerve has both afferent (sensory) and efferent (motor) fibers, allowing it to transmit signals bidirectionally between the gut and the brain.
Here’s how the vagus nerve relates to poor gut health:
- Gut-Brain Axis: The vagus nerve is a major component of the gut-brain axis, a bidirectional communication system that links the gut and the central nervous system (CNS). Signals sent via the vagus nerve from the gut can influence brain function and vice versa. This communication pathway plays a crucial role in regulating various physiological processes, including digestion, mood, stress response, and immune function.
- Regulation of Digestion: The vagus nerve innervates many organs involved in digestion, including the stomach, small intestine, and colon. It helps regulate gastric motility, secretion of digestive enzymes, and nutrient absorption. Dysfunction of the vagus nerve can lead to dysregulation of these processes, contributing to digestive issues such as delayed gastric emptying, bloating, constipation, or diarrhea.
- Immune Function: The vagus nerve also plays a role in modulating immune responses in the gut. It can interact with immune cells in the gut-associated lymphoid tissue (GALT) and regulate inflammation and immune activation. Dysfunction of the vagus nerve may disrupt this immune modulation, leading to chronic inflammation and immune-related gut disorders.
- Stress Response: The vagus nerve is involved in the regulation of the stress response through its connection with the hypothalamic-pituitary-adrenal (HPA) axis. Activation of the vagus nerve can promote relaxation and dampen the stress response, while dysfunction of the vagus nerve may contribute to heightened stress levels and dysregulated cortisol production, which can negatively impact gut health.
- Microbiota-Gut-Brain Axis: The vagus nerve is also involved in the bidirectional communication between the gut microbiota and the brain, known as the microbiota-gut-brain axis. It can transmit signals generated by gut microbiota activity to the brain, influencing mood, behavior, and cognitive function. Dysfunction of the vagus nerve may disrupt this communication, potentially contributing to mood disorders such as anxiety and depression, which are often associated with poor gut health.
Overall, dysfunction of the vagus nerve can contribute to poor gut health through dysregulation of digestion, immune function, stress response, and microbiota-brain communication. Maintaining vagal tone and supporting vagal nerve function through lifestyle interventions such as stress management, regular physical activity, and relaxation techniques may help promote optimal gut health.
How to heal and rebuild your gut wall lining?
Promoting mucosal healing involves supporting the repair and regeneration of the mucous membranes that line the gastrointestinal tract. Here are some nutrients and compounds that have been shown to support mucosal healing, along with dietary sources and considerations for supplementation:
- Butyrate:
- Source: Butyrate is a short-chain fatty acid produced by the fermentation of dietary fibers in the colon. It is also found in butter and ghee (clarified butter).
- Function: Butyrate serves as a primary energy source for the cells lining the colon (colonocytes) and plays a crucial role in maintaining gut barrier function, reducing inflammation, and promoting mucosal healing.
- Considerations: Increasing dietary fiber intake, particularly from sources like fruits, vegetables, whole grains, and legumes, can support butyrate production by gut bacteria. Butyrate supplements are also available but should be used under the guidance of a healthcare provider.
- Quercetin:
- Sources: Quercetin is a flavonoid found in various plant foods, including onions, apples, citrus fruits, berries, leafy greens, and broccoli.
- Function: Quercetin possesses antioxidant, anti-inflammatory, and immune-modulating properties. It has been shown to support gut health by reducing inflammation, stabilizing mast cells, and promoting tissue repair.
- Considerations: Consuming a diet rich in quercetin-containing foods can help support mucosal healing. Quercetin supplements are available but should be used cautiously, especially in high doses, and under the guidance of a healthcare provider.
- Glutathione:
- Sources: Glutathione is a tripeptide composed of three amino acids: cysteine, glutamate, and glycine. It is found in various foods, including fruits, vegetables, lean meats, fish, and dairy products. Additionally, foods rich in sulfur-containing amino acids, such as cysteine and methionine, can support endogenous glutathione production.
- Function: Glutathione is a potent antioxidant that helps protect cells from oxidative damage and supports detoxification processes. It also plays a critical role in immune function and tissue repair.
- Considerations: Consuming a balanced diet rich in fruits, vegetables, and quality protein sources can provide the building blocks necessary for glutathione synthesis. In some cases, supplementation with glutathione precursors (such as N-acetylcysteine) or liposomal glutathione may be beneficial, but it’s important to consult with a healthcare provider for proper dosing and monitoring.
Incorporating a variety of nutrient-rich foods into your diet can help promote mucosal healing and support overall gut health. However, supplementation should be approached cautiously and under the guidance of a qualified healthcare provider, especially if you have specific health concerns or medical conditions.
Head to www.debbiepotts.net to schedule a call to discover more plus check out options on Fullscript here
Don’t forget to test for Anti-LPS or endotoxicity!

