What is METABOLIC SYNDROME?
Metabolic syndrome is a cluster of risk factors that increase the likelihood of developing cardiovascular disease, type 2 diabetes, and other health problems. It is not a disease itself but a combination of several conditions and lifestyle factors that, when present together, significantly raise the risk of these chronic diseases.
The specific criteria for diagnosing metabolic syndrome may vary slightly between different medical organizations and guidelines, but the following are common components:
- Abdominal obesity: Typically measured by waist circumference. For example, a waist circumference of over 40 inches (102 cm) in men or over 35 inches (88 cm) in women is often considered a risk factor.
- Elevated blood pressure: Blood pressure readings equal to or higher than 130/85 mm Hg or the use of blood pressure-lowering medication.
- Elevated fasting blood sugar: A fasting blood glucose level of 100 mg/dL (5.6 mmol/L) or higher. INSULIN should be 1 – 5 µIU/mL
- Elevated triglycerides: A blood triglyceride level of 150 mg/dL (1.7 mmol/L) or higher.
- Low high-density lipoprotein (HDL) cholesterol: HDL cholesterol levels below 40 mg/dL (1.04 mmol/L) in men or below 50 mg/dL (1.3 mmol/L) in women.
Functional medicine is an approach to healthcare that focuses on addressing the root causes of health problems rather than just treating symptoms. It takes a holistic view of a person’s health and often involves personalized, integrative therapies.
Reversing metabolic syndrome in functional medicine typically involves addressing the underlying factors contributing to the condition.
Here are some steps that may be considered in a functional medicine approach to reversing metabolic syndrome:
- Comprehensive Assessment: Functional medicine practitioners often conduct a thorough assessment of your health history, genetics, lifestyle, and environmental factors to identify the specific causes and triggers of metabolic syndrome in your case.
- Personalized Nutrition: A functional medicine approach emphasizes individualized dietary plans tailored to your unique needs. This may involve identifying food sensitivities, allergies, and deficiencies and creating a personalized nutrition plan that focuses on whole, unprocessed foods.
- Balancing Blood Sugar: Controlling blood sugar levels is a key component of managing metabolic syndrome. Functional medicine may involve using dietary changes, including low-glycemic foods, and possibly intermittent fasting to help stabilize blood sugar levels.
- Managing Inflammation: Chronic inflammation is often associated with metabolic syndrome. Functional medicine practitioners may recommend anti-inflammatory diets, supplements, and lifestyle changes to reduce inflammation.
- Stress Management: Chronic stress can contribute to metabolic syndrome. Stress-reduction techniques such as mindfulness meditation, yoga, and deep breathing exercises may be recommended to manage stress and improve metabolic health.
- Exercise and Physical Activity: Functional medicine encourages regular physical activity as part of a holistic approach to health. Exercise can help improve insulin sensitivity, reduce abdominal fat, and lower blood pressure.
- Sleep Optimization: Adequate and quality sleep is crucial for metabolic health. Functional medicine practitioners may address sleep issues and recommend strategies to improve sleep quality.
- Supplements and Nutraceuticals: Depending on your individual needs, functional medicine practitioners may recommend specific supplements or nutraceuticals to address nutritional deficiencies or support metabolic health.
- Detoxification: Some functional medicine approaches include detoxification protocols to help the body eliminate toxins and promote overall health.
- Patient Education and Empowerment: Functional medicine practitioners often place a strong emphasis on educating patients about their condition and empowering them to take an active role in their health through lifestyle changes.
It’s important to note that while functional medicine can offer a comprehensive and individualized approach to metabolic syndrome, it should be done under the guidance of a qualified healthcare provider, such as a functional medicine practitioner or integrative medicine specialist.
These practitioners can work with you to create a personalized treatment plan that addresses your specific needs and goals while considering your overall health and well-being.
Additionally, it’s essential to follow up regularly with your healthcare provider to monitor progress and make adjustments to your treatment plan as needed.
In functional medicine, inflammatory markers are specific substances or measurements used to assess the presence and extent of inflammation in the body.
Chronic inflammation is believed to play a significant role in the development of various chronic diseases and conditions, including metabolic syndrome, autoimmune diseases, cardiovascular diseases, and more. Functional medicine practitioners use these markers to identify underlying causes of inflammation and guide treatment strategies.
Some common inflammatory markers in functional medicine include:
- C-reactive protein (CRP): CRP is a protein produced by the liver in response to inflammation. High levels of CRP in the blood can indicate acute or chronic inflammation. It is often measured as a high-sensitivity CRP (hs-CRP) test, which is more sensitive for detecting low levels of inflammation.
- Erythrocyte sedimentation rate (ESR or sed rate): ESR measures how quickly red blood cells settle at the bottom of a test tube. A high ESR can suggest the presence of inflammation, but it is not specific and can be influenced by other factors.
- Fibrinogen: Fibrinogen is a protein involved in blood clotting and inflammation. Elevated levels of fibrinogen can indicate inflammation and an increased risk of cardiovascular disease.
- Homocysteine: High levels of homocysteine in the blood are associated with inflammation and an increased risk of cardiovascular disease. Functional medicine practitioners may assess homocysteine levels to evaluate cardiovascular health.
- Proinflammatory cytokines: Cytokines are small proteins that play a key role in cell signaling during the immune response. Proinflammatory cytokines, such as interleukin-6 (IL-6), interleukin-1 beta (IL-1β), and tumor necrosis factor-alpha (TNF-α), are often measured to assess systemic inflammation.
- Oxidative stress markers: Oxidative stress occurs when there is an imbalance between the production of reactive oxygen species (free radicals) and the body’s ability to neutralize them. Functional medicine may involve measuring markers such as malondialdehyde (MDA) or 8-hydroxydeoxyguanosine (8-OHdG) to assess oxidative stress.
- Adipokines: These are cytokines produced by fat cells (adipose tissue). Dysregulation of adipokines can contribute to inflammation and metabolic dysfunction. Leptin and adiponectin are examples of adipokines that may be measured.
- Markers of gut health: Functional medicine often considers the gut’s role in inflammation. Tests may include measuring markers like zonulin to assess intestinal permeability (“leaky gut”) or evaluating gut microbiota composition.
- Food sensitivity testing: Some functional medicine approaches involve identifying food sensitivities or allergies through blood tests, as certain foods can trigger inflammatory responses in susceptible individuals.
- Genetic testing: Genetic factors can influence an individual’s susceptibility to inflammation and chronic diseases. Functional medicine practitioners may use genetic testing to assess genetic predispositions related to inflammation and tailor interventions accordingly.
These inflammatory markers are used in functional medicine to create a comprehensive picture of an individual’s inflammatory status and overall health. Based on the results, functional medicine practitioners can develop personalized treatment plans that address the underlying causes of inflammation and promote health and wellness. It’s important to work with a qualified healthcare provider or functional medicine practitioner when interpreting and addressing these markers to ensure a safe and effective approach to health optimization.

How can a PNOE Resting Metabolic Analysis provide clues to your Metabolic Health?
How can you prevent metabolic syndrome?
Here’s how a PNOE Resting Metabolism Analysis can help:
- Resting Metabolic Rate (RMR) Assessment: PNOE measures an individual’s resting metabolic rate, which is the amount of energy (calories) your body needs at rest to maintain basic functions like breathing, circulation, and cell repair. Understanding your RMR can help you determine your daily caloric needs and guide dietary recommendations to support weight management.
- Identification of Energy Imbalances: By comparing your actual caloric intake to your RMR, you can identify if you’re consuming too many or too few calories. Consistently overeating can lead to weight gain and increased metabolic syndrome risk, while chronic undereating can impact metabolic health negatively.
- Metabolic Efficiency Assessment: PNOE can provide information on how efficiently your body is utilizing carbohydrates and fats for energy. This information can be used to create a personalized diet plan that optimizes macronutrient ratios to improve metabolic health.
- Nutrient Recommendations: Based on your metabolic analysis, PNOE can suggest specific dietary changes to improve metabolic health. This might include recommendations for carbohydrate intake, dietary fats, protein, and meal timing.
- Exercise Recommendations: PNOE analysis can help identify the most effective exercise intensity and duration for your metabolism. It can guide personalized fitness plans to improve insulin sensitivity, increase muscle mass, and promote fat loss.
- Tracking Progress: Regular PNOE assessments can track changes in your metabolic parameters over time, helping you monitor the effectiveness of your lifestyle changes and interventions in improving metabolic health.
- Motivation and Accountability: Knowing your metabolic parameters and receiving personalized recommendations can motivate individuals to make positive lifestyle changes and stick to their health and wellness goals.
It’s important to note that while a PNOE Resting Metabolism Analysis can provide valuable insights, it is just one tool in the overall assessment of metabolic health. To prevent or manage metabolic syndrome effectively, a comprehensive approach that includes a thorough medical evaluation, regular physical activity, a balanced diet, stress management, and adequate sleep is recommended.
Individuals interested in using PNOE or similar metabolic analyzers should work with qualified healthcare professionals or registered dietitians who can interpret the results and help create personalized plans based on the metabolic data.
Additionally, it’s crucial to consider other risk factors and aspects of metabolic health beyond resting metabolism, such as blood pressure, blood glucose, lipid levels, and waist circumference, as part of a holistic approach to metabolic syndrome prevention and management.
What does the PNOE Resting Metabolism Test tell you?
PNOE Resting Metabolism Analysis:
Metabolic Fitness
- It’s a gauge of how well your body converts nutrients (e.g., fats and carbohydrates) into the energy it needs to move and sustain its vital functions (e.g., brain, heart, and lung function).
- The metabolic fitness score is calculated by combining the resting metabolic rate and the fat-urning efficiency scores.
Resting Metabolic Rate
- The resting metabolic rate score is a gauge of how fast or slow your metabolism is.
- Whether your body is burning more or fewer calories than what’s predicted based on your weight, gender, age, and height.
- It’s calculated by comparing the resting metabolic rate measured by the device with the estimated value generated by the Harris-Benedict equation.
- The Harris Benedict RMR value is calculated based on your age, gender, weight, and height and is referred to as the “predicted” metabolic rate.
Fat-Burning Efficiency
- It represents the ability to ‘’burn’’ fat as a fuel source at rest.
- Resting RER values closer to 0.7 reflect a high-fat burning efficiency score, whereas resting RER values closer to 1.0 reflect a low-fat burning efficiency score.
Heart Fitness
- It’s a gauge of your cardiovascular system’s fitness and a risk factor for heart-related conditions.
- t’s assessed by analyzing heart rate variability biomarkers such as Low and High-Frequency bands.
Lung Fitness
- It’s a gauge of your lungs’ condition and a risk factor for respiratory-related conditions.
- It’s calculated based on the tidal volume (i.e. the amount of air exhaled in each breath) measured during the test.
- A reduced tidal volume is a risk factor for developing lung conditions.
Breathing & Cognition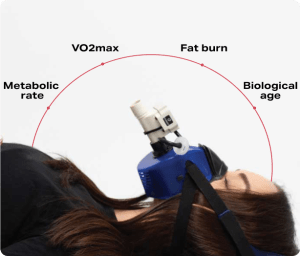
- It reflects how breathing affects a person’s ability to think and perform cognitive tasks.
- It’s calculated based on breathing frequency at rest.
- Breathing faster than a specific threshold is an indication of hyperventilation, a state that reduces oxygenation to the brain and the ability to perform cognitive tasks.
Breathing & Posture
- It’s a gauge of how your breathing affects posture, the likelihood of musculoskeletal injury, and lower back pain.
- The breathing and posture score is calculated based on your resting breathing frequency.
Metabolic Disease Risk
- It’s a risk factor for developing metabolic-related issues
- It’s calculated based on your ability to utilize fat at rest.
- The lower the RER, the higher your fat-burning efficiency and the lower your metabolic disease risk score.
Calories Balance- Fuel Sources
- Your body uses a mixture of carbs and fats to produce the energy needed to sustain life and power daily activities.
- High reliance on fat as a fuel source is one of the most reliable indicator of good cellular condition and is strongly associated with low likelihood of weight gain or weight regain.
- Macronutrient balance based on Nutritional Therapy Assessment + PNOE Assessment
Nutritional Therapy Assessment
-
- Nutritional Therapy: Nutritional therapy is a holistic approach to health and well-being that focuses on using food and nutrition to support overall health and address specific health concerns or conditions. It often involves working with a trained nutritional therapist or practitioner who assesses an individual’s dietary habits, lifestyle, and health goals.
- Assessment: A nutritional therapy assessment typically involves gathering information about an individual’s:
- Dietary Habits: This includes the types of foods a person eats, portion sizes, meal timing, and any dietary restrictions or preferences.
- Health History: Information about a person’s medical history, current health conditions, medications, and supplements.
- Lifestyle Factors: Factors such as physical activity, stress levels, sleep patterns, and daily routines can impact nutrition and health.
- Goals and Concerns: Identifying an individual’s specific health goals or concerns is crucial to tailoring a nutritional plan.
- NutriQ: NutriQ is a specific tool to gather detailed information about an individual’s signs and symptoms then correlate to functional lab tests and other assessments.
- Food, Activity & Mood Log Assessment- 3 day journal tracking food, mood, motility, hydration, supplements, exercise and sleep!
What is Metabolic Syndrome? How can you prevent it?

While PNOE Metabolic testing can provide valuable information for optimizing health and reducing the risk factors associated with metabolic syndrome, it should be considered as part of a broader health and wellness program. It is essential to work with healthcare professionals, such as registered dietitians, exercise physiologists, or physicians, to interpret the results and create a comprehensive plan for metabolic health.
Ultimately, preventing metabolic syndrome involves a multifaceted approach that includes maintaining a healthy diet, engaging in regular physical activity, managing stress, getting adequate sleep, and avoiding smoking and excessive alcohol consumption. PNOE Metabolic testing can be a useful tool to personalize and fine-tune these lifestyle choices based on an individual’s unique metabolic profile.
To be diagnosed with metabolic syndrome, an individual typically needs to meet at least three of these criteria. The presence of metabolic syndrome is associated with an increased risk of cardiovascular disease, stroke, and type 2 diabetes.
Testing for metabolic syndrome involves assessing these individual components through various medical tests and measurements. If you meet the criteria for metabolic syndrome, it’s essential to work with a healthcare provider to manage and address these risk factors. Lifestyle changes, such as adopting a healthy diet, engaging in regular physical activity, quitting smoking, and managing stress, are often recommended to reduce the risk and improve overall health. In some cases, medications may also be prescribed to manage individual components of metabolic syndrome, such as high blood pressure or high cholesterol.
Regular follow-up with a healthcare provider is crucial to monitor progress and make necessary adjustments to the treatment plan. Managing metabolic syndrome can significantly reduce the risk of serious health complications.
Let’s be health optimizers and preventative!
Remember… the specific criteria for diagnosing metabolic syndrome may vary slightly between different medical organizations and guidelines, but the following are common components:
- Abdominal obesity: Typically measured by waist circumference. For example, a waist circumference of over 40 inches (102 cm) in men or over 35 inches (88 cm) in women is often considered a risk factor.
- Elevated blood pressure: Blood pressure readings equal to or higher than 130/85 mm Hg or the use of blood pressure-lowering medication.
- Elevated fasting blood sugar: A fasting blood glucose level of 100 mg/dL (5.6 mmol/L) or higher.
- Elevated triglycerides: A blood triglyceride level of 150 mg/dL (1.7 mmol/L) or higher.
- Low high-density lipoprotein (HDL) cholesterol: HDL cholesterol levels below 40 mg/dL (1.04 mmol/L) in men or below 50 mg/dL (1.3 mmol/L) in women.
- Ranges in our Functional Ranges for Lipid …
- Cholesterol 170-200
- Triglycerides 70-80
- HDL Cholesterol 55-85
- LDL Cholesterol 80-100
- Trig:HDL Ratio 0-2
- TC/HDL Ratio
Blood Chemistry Markers including
-
-
- Fasting Glucose
- A1C
- Insulin
- CRP
- Triglycerides
-
Body Composition Testing
-
-
- Total Weight
- Lean body mass/fat free mass
- Fat Mass
- Waist measurements
- Hip measurements
-
PNOE Metabolism
-
-
-
- Resting metabolism rate – calories at rest, Metabolic Efficiency- Fat Burn Efficiency, Metabolic Disease Risk
- Analyze how fast or slow your metabolism is, determine the optimal calorie intake for your goal, and measure how effectively your cells burn fats and carbohydrates at rest and during exercise. This information may also reveal the risk for metabolic disorders such as Type II Diabetes.
- Analyze how effectively your cells utilize oxygen, burn fat as a fuel source, and clear fatigue metabolites during exercise. This information is also used to determine the optimal macro intake during exercise.
- Analyze your cardiovascular and lung fitness with lab-grade accuracy and understand how these vital organs impact your health and well-being. Your lung fitness is evaluated through four distinct metrics that paint one of the most complete pictures of how fit your lungs are and how well you utilize them.
- Analyze how your breath affects cognitive performance, lower back pain, and myoskeletal health. Breathing is one of the most vital functions for maintaining high levels of brain activity and avoiding injuries such as lower back pain.
- Analyze your biological age as well as how long and well you are estimated to live. According to the American Heart Association this test provides the most reliable and accurate measure of longevity and mortality risk.
-
-

