 Functional medicine markers for chronic inflammation, cardiovascular disease, metabolic health, and longevity can vary, but here are some common ones:
Functional medicine markers for chronic inflammation, cardiovascular disease, metabolic health, and longevity can vary, but here are some common ones:
Chronic Inflammation:
- C-reactive protein (CRP): Elevated levels of CRP indicate inflammation in the body.
- Erythrocyte sedimentation rate (ESR): Higher ESR levels can indicate inflammation.
- Tumor necrosis factor-alpha (TNF-alpha): Elevated levels are associated with inflammation.
- Interleukin-6 (IL-6): Higher levels can indicate chronic inflammation.
- Homocysteine levels: Elevated levels may indicate inflammation and increased risk for cardiovascular disease.
- Oxidative stress markers: Such as malondialdehyde (MDA) or F2-isoprostanes.
Cardiovascular Disease:
- Lipid profile: Including total cholesterol, LDL cholesterol, HDL cholesterol, and triglycerides.(see below for ideal markers)
- High sensitivity C-reactive protein (hs-CRP): Indicates inflammation and is a risk factor for cardiovascular disease.
- Blood pressure: Elevated blood pressure is a risk factor for cardiovascular disease.
- Homocysteine levels: Elevated levels can be associated with increased cardiovascular risk.
- Hemoglobin A1c (HbA1c): Elevated levels indicate poor glycemic control and are associated with increased cardiovascular risk.
- Plaque markers: Such as coronary artery calcium (CAC) score or carotid intima-media thickness (CIMT).
Functional lab tests for assessing lipid profile, heart disease risk, cardiovascular risk, and metabolic health typically include:
- Total Cholesterol: This measures the total amount of cholesterol in your blood. However, it doesn’t give a complete picture of heart disease risk by itself.
- LDL Cholesterol (Low-Density Lipoprotein): Often referred to as “bad” cholesterol, high levels of LDL cholesterol can lead to plaque buildup in the arteries, increasing the risk of heart disease.
- HDL Cholesterol (High-Density Lipoprotein): Known as “good” cholesterol, higher levels of HDL cholesterol are associated with a lower risk of heart disease because it helps remove LDL cholesterol from the arteries.
- Triglycerides: Elevated triglyceride levels can also increase the risk of heart disease, especially when combined with low HDL cholesterol and high LDL cholesterol.
- Non-HDL Cholesterol: This includes all the cholesterol carried by LDL particles plus lipoprotein (a) and other atherogenic lipoproteins. Non-HDL cholesterol is considered a better predictor of cardiovascular risk than LDL cholesterol alone.
- Apolipoprotein B (ApoB): ApoB is the main apolipoprotein of LDL cholesterol particles and is a marker of the total number of atherogenic lipoprotein particles. Elevated ApoB levels are associated with increased cardiovascular risk.
- Apolipoprotein A-I (ApoA-I): ApoA-I is the main apolipoprotein of HDL cholesterol particles. Higher levels of ApoA-I are associated with a decreased risk of cardiovascular disease.
- Lipoprotein (a) [Lp(a)]: Elevated levels of Lp(a) are an independent risk factor for cardiovascular disease.
- Small Dense LDL (sdLDL): This type of LDL particle is smaller and denser than normal LDL particles and is more atherogenic.
- LDL Particle Number (LDL-P): This measures the number of LDL particles in the blood, which is considered a better predictor of cardiovascular risk than LDL cholesterol levels alone.
- Oxidized LDL (oxLDL): Oxidized LDL particles are more likely to contribute to the development of atherosclerosis.
- Fasting Insulin: High insulin levels can indicate insulin resistance, which is associated with an increased risk of heart disease and metabolic disorders.
- HbA1c (Glycated Hemoglobin): This measures the average blood sugar levels over the past 2-3 months and can indicate the risk of developing diabetes or insulin resistance, both of which are risk factors for heart disease.
- C-reactive Protein (CRP): Elevated levels of CRP indicate inflammation, which plays a significant role in the development of atherosclerosis and heart disease.
- Homocysteine: Elevated levels of homocysteine are associated with an increased risk of cardiovascular disease.
Metabolic Health:
- Fasting blood glucose: Elevated levels may indicate insulin resistance and metabolic dysfunction.
- Insulin levels: High fasting insulin levels or impaired glucose tolerance indicate insulin resistance.
- Hemoglobin A1c (HbA1c): Reflects average blood sugar levels over the past 2-3 months.
- Lipid profile: High levels of LDL cholesterol and triglycerides, and low levels of HDL cholesterol may indicate metabolic dysfunction.
- Waist circumference: Increased waist circumference is associated with metabolic syndrome and insulin resistance.
- Liver function tests: Elevated liver enzymes (ALT, AST) may indicate fatty liver disease, which is closely linked to metabolic health.
Longevity:
- Telomere length: Shortened telomeres are associated with aging and age-related diseases.
- Inflammatory markers: High levels of inflammation are associated with accelerated aging and reduced longevity.
- Insulin sensitivity: Better insulin sensitivity is associated with increased longevity.
- Nutrient levels: Adequate levels of antioxidants, vitamins, and minerals support longevity.
- Body composition: Healthy body composition, with lower levels of body fat and higher lean muscle mass, is associated with increased longevity.
- Physical fitness: Higher levels of physical activity and fitness are correlated with increased longevity.
These markers are often assessed in conjunction with clinical symptoms and other diagnostic tests to provide a comprehensive picture of an individual’s health status. It’s important to work with a healthcare provider or practitioner knowledgeable in functional medicine to interpret these markers and develop an appropriate treatment plan

In functional lab testing for longevity, cardiovascular risk, and heart health, the lipid panel is a crucial set of markers to assess. Here are the markers typically included in a lipid panel, along with optimal ranges for functional medicine values and explanations of their importance for cardiovascular health, metabolic health, and longevity.
Here are more current markers used in functional lab testing for heart disease risk assessment, along with their optimal values and purposes:
-
Apolipoprotein B (ApoB):
- Optimal Range: < 90 mg/dL
- Purpose: ApoB reflects the number of atherogenic particles (LDL, VLDL) in the blood and is considered a better indicator of cardiovascular risk than LDL cholesterol alone. Elevated levels of ApoB are associated with increased risk of atherosclerosis and heart disease.
-
Apolipoprotein A-I (ApoA-I):
- Optimal Range: > 120 mg/dL
- Purpose: ApoA-I is the main protein component of HDL particles. Higher levels of ApoA-I are associated with increased reverse cholesterol transport, promoting the removal of cholesterol from arteries and reducing the risk of atherosclerosis and cardiovascular events.
-
ApoB/ApoA-I Ratio:
- Optimal Range: < 0.8
- Purpose: This ratio reflects the balance between atherogenic (ApoB-containing) and anti-atherogenic (ApoA-I-containing) lipoproteins. A lower ratio indicates a healthier lipid profile and reduced cardiovascular risk.
-
Lipoprotein(a) [Lp(a)]:
- Optimal Range: < 30 mg/dL
- Purpose: Elevated levels of Lp(a) are an independent risk factor for cardiovascular disease. Lp(a) promotes atherosclerosis by interfering with the breakdown of blood clots and promoting inflammation in arterial walls.
-
Small Dense LDL (sdLDL) Particles:
- Optimal Range: < 20 mg/dL
- Purpose: sdLDL particles are more atherogenic than larger LDL particles and are associated with increased cardiovascular risk. Measuring sdLDL levels provides insight into the quality of LDL particles and helps identify individuals at higher risk of heart disease.
-
Omega-3 Index:
- Optimal Range: > 8%
- Purpose: The omega-3 index reflects the percentage of EPA (eicosapentaenoic acid) and DHA (docosahexaenoic acid) in red blood cell membranes. Higher omega-3 levels are associated with reduced inflammation, improved lipid profiles, and decreased risk of cardiovascular events.
Purpose of These Markers:
- Enhanced Risk Assessment: These markers offer a more comprehensive assessment of cardiovascular risk beyond traditional lipid parameters. By evaluating the quantity, quality, and functionality of lipoproteins, they provide deeper insights into an individual’s risk profile.
- Personalized Treatment Approach: By identifying specific lipid abnormalities and underlying metabolic imbalances, functional testing allows for targeted interventions tailored to the individual’s unique risk factors and health goals.
- Prevention and Intervention: Monitoring these markers enables early detection of cardiovascular risk, allowing for proactive interventions to optimize lipid metabolism, reduce inflammation, and mitigate the progression of atherosclerosis, ultimately promoting heart health and longevity.
Functional lab testing with these markers empowers healthcare providers to take a proactive approach to cardiovascular health, focusing not only on cholesterol levels but also on underlying metabolic and inflammatory factors that contribute to heart disease risk. This personalized approach facilitates the development of targeted interventions aimed at optimizing lipid metabolism and promoting cardiovascular wellness.
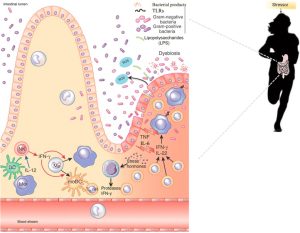
Do you have clues of a LEAKY GUT?
Functional lab testing can provide valuable insights into the signs and symptoms of leaky gut syndrome, also known as increased intestinal permeability. Here are some common markers used in functional medicine to assess and identify leaky gut:
-
Zonulin:
- Purpose: Zonulin is a protein that regulates intestinal permeability.
- Elevated levels of zonulin indicate increased intestinal permeability, suggesting leaky gut syndrome.
-
Lactulose/Mannitol Test:
- Purpose: This test involves measuring the levels of lactulose and mannitol in urine after oral administration.
- Increased urinary excretion of lactulose and decreased excretion of mannitol suggest increased intestinal permeability.
-
Intestinal Permeability Assay (e.g., Cyrex Array 2):
- Purpose: This assay measures the levels of antibodies against various tight junction proteins, such as occludin and zonulin, which are involved in maintaining intestinal barrier function.
- Elevated levels of these antibodies indicate disruption of tight junctions and increased intestinal permeability.
-
Anti-Saccharomyces cerevisiae Antibodies (ASCA) and Anti-Saccharomyces cerevisiae mannans (ASCA-M):
- Purpose: These antibodies are associated with Crohn’s disease and other inflammatory bowel diseases (IBD).
- Elevated levels may suggest immune system activation and intestinal barrier dysfunction.
-
Fecal Calprotectin:
- Purpose: Calprotectin is a marker of intestinal inflammation.
- Elevated levels of fecal calprotectin suggest mucosal inflammation, which can be indicative of underlying gut dysfunction, including leaky gut.
-
Short-Chain Fatty Acids (SCFAs):
- Purpose: SCFAs are produced by gut bacteria during the fermentation of dietary fiber.
- Low levels of SCFAs may indicate dysbiosis (imbalance of gut microbiota) and impaired gut barrier function, contributing to leaky gut syndrome.
-
Food Sensitivity Testing:
- Purpose: Identifying food sensitivities and intolerances can be helpful in managing leaky gut syndrome.
- IgG and IgA antibody testing can help identify immune reactions to specific foods, which may contribute to gut inflammation and permeability.
Purpose of These Markers:
- Assessment of Intestinal Barrier Function: These markers provide insights into the integrity of the intestinal barrier and the degree of permeability. Elevated levels or abnormal patterns of these markers suggest dysfunction in the gut barrier, which may contribute to leaky gut syndrome.
- Identification of Underlying Causes: Testing for antibodies against specific tight junction proteins, microbial antigens, and inflammatory markers helps identify potential triggers and underlying factors contributing to leaky gut, such as dysbiosis, inflammation, and immune dysregulation.
- Personalized Treatment Approach: By identifying specific dysfunctions in the gut barrier and underlying triggers, functional testing allows for targeted interventions aimed at restoring gut health, reducing inflammation, and promoting healing of the intestinal mucosa.
- Monitoring Treatment Progress: Periodic retesting of these markers can help monitor the effectiveness of interventions and track improvements in gut barrier function and overall gastrointestinal health over time.
Functional lab testing for leaky gut syndrome provides valuable information for healthcare providers to develop personalized treatment plans that address the underlying causes and promote healing of the gut mucosa, ultimately improving digestive health and overall well-being.
