First of all… What is LEAKY GUT?
What is Leaky Gut Syndrome?
Leaky gut syndrome (also known as increased intestinal permeability) is a term used by experienced leaky gut doctors in Tampa to describe the condition of the intestines when its lining becomes damaged and gaps appear between the cells.
These gaps allow large particles and toxins to pass through the intestinal wall and escape into the body. Because these “foreign objects” are not supposed to be in the blood they trigger the immune system, which sets up inflammation in different parts of the body and a cascade of symptoms such as headaches, fatigue, brain fog, food sensitivities, bloating, cramps, and more.
Leaky gut is not widely recognized by mainstream physicians but as Dr. Oz recently mentioned, it is often overlooked because conventional medicine doesn’t know how to diagnose it, and a patient can present with multiple, seemingly unrelated symptoms.
Because a leaky gut is responsible for so many unexplained chronic health conditions, it is one of the first things we test for and address. Repairing a leaky gut is one of the most important foundational steps to recover from any chronic disease.
Leaky Gut Symptoms
Leaky gut often causes uncomfortable pains, sensations, feelings, and symptoms in other parts of the body. Patients can feel fatigued, have brain fog, feel depressed, have unexplained pains or even an overactive immune system.
Common leaky gut symptoms include:
- stomach gas and bloating
- acid reflux / heartburn
- joint pains
- unexplained pains
- brain fog
- fatigue and lethargy
- diagnosis of chronic fatigue or fibromyalgia
- an autoimmune disease
- seasonal allergies or asthma
- hormone imbalances
- anxiety or depression
- skin issues
- candida
- food allergies
- and many more
Causes of Leaky Gut
Many factors are implicated such as:
- nutritional deficiencies
- poor diet
- eating irritating foods
- food sensitivities
- amino acid deficiencies
- chronic stress
- environmental toxins
- pesticides
- chemicals & additives
- GMO foods
- inflammation
- autoimmunity
- systemic toxicity
- yeast
- fungi
- mold
- bacterial overgrowth
- antibiotics and certain medications
Natural Leaky Gut Treatment
If you are found to have a leaky gut, our top gut doctor will prescribe a natural leaky gut treatment program which will be developed to address the underlying reason(s) why you developed it.
Depending on the underlying causes and your current situation, treatment may include one or more of the following:
- balancing the gut microbiome
- antifungals to kill off fungus or mold
- ozone therapy to kill off of any bad bugs, microbes, etc.
- treating and healing any autoimmunity
- resolving any hidden infections, etc. that would have triggered the autoimmunity
- calming an overactive immune system
- detoxifying any heavy metals, toxins, or chemicals
- food allergy detection & elimination
- healing the gut lining
- IV Therapies to speed gut healing
- thermal heat treatments
- HBOT (hyperbaric oxygen therapy) to speed healing
- PEMF to speed healing
- prebiotics & probiotics to re-innoculate the gut
- boosting mitochondrial function, to speed healing
- any needed dietary modifications
- enzymes & HCL as needed short-term, to support digestion
- high quality targeted supplements to provide the gut raw materials to heal
Part of your natural leaky gut treatment will include resolving any secondary damage caused by having a leaky gut.
Don’t Put off Addressing Gut Dysfunction
Getting your gut health on-point and healing any outstanding issues should not be put on the back burner. Gut health issues, like leaky gut, affect all areas of your health. Your gut is the foundation for the strength and proper function of your immune system. In addition it plays a vital role in nutrient absorption, waste elimination, energy production, and brain health.
Gut issues that are left untreated tend to develop into more serious issues, like autoimmune conditions, Crohn’s, IBS, arthritis, joint pains, neurological disorders, and even cardiovascular disease.
What can seem like a minor gut annoyance, if left untreated, over time can snowball into a more serious condition. Don’t let that be you. Get it checked and fix it while it’s easy and cost-effective to do so.
https://www.lifeworkswellnesscenter.com/how-to-heal-your-gut-naturally/what-is-leaky-gut-syndrome.html
What is LPS?

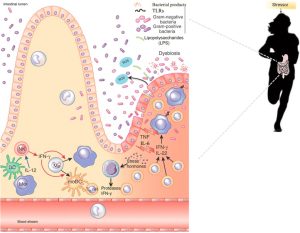
LPS stands for Lipopolysaccharide. It’s a molecule found in the outer membrane of Gram-negative bacteria, which are a type of bacteria characterized by the structure of their cell walls. LPS is considered an endotoxin because it’s released when these bacteria die and their cell walls break down.
Dr. Tom O’Bryan talks about Leaky Gut & LPS…
Excessive Lipopolysaccharides (LPS). LPS is a type of endotoxin produced inside your body.
LPS is like a poison. Small amounts in your bloodstream trigger the production of an anti-inflammatory hormone, adiponectin.
That’s great!
But LPS is the perfect example of too much of a good thing.
Too much actually creates inflammation.
If it stays in the gut, it isn’t a huge issue.
But with leaky gut, it triggers inflammation in the body when it enters the bloodstream
What are gram negative bacteria?
- Gram-negative bacteria are a group of bacteria that have a distinct cell wall structure, which includes an outer membrane composed of lipopolysaccharides.
- This outer membrane acts as a protective barrier for the bacteria and helps them to survive in various environments.
- LPS molecules consist of a lipid portion (lipid A), a core polysaccharide, and an O-specific polysaccharide chain.
- LPS plays a crucial role in the structural integrity of Gram-negative bacteria and also serves as an endotoxin when released into the environment or bloodstream, triggering immune responses in animals and humans.
Gram-negative bacteria are a diverse group of bacteria that possess a characteristic cell wall structure that stains pink or red in the Gram staining method.
Some common examples of Gram-negative bacteria include:
- Escherichia coli (E. coli): Found in the intestines of humans and animals, some strains can cause gastrointestinal infections.
- Salmonella spp.: Pathogenic strains can cause foodborne illnesses such as salmonellosis.
- Pseudomonas aeruginosa: An opportunistic pathogen that can cause infections in wounds, burns, and the respiratory system, particularly in immunocompromised individuals.
- Klebsiella pneumoniae: Known for causing pneumonia and urinary tract infections, especially in hospital settings.
- Neisseria gonorrhoeae: The causative agent of gonorrhea, a sexually transmitted infection.
- Neisseria meningitidis: Can cause meningitis and septicemia.
- Vibrio cholerae: The bacterium responsible for cholera, a diarrheal disease transmitted through contaminated water and food.
- Helicobacter pylori: Associated with gastritis, peptic ulcers, and an increased risk of stomach cancer.
- Bordetella pertussis: Causes whooping cough (pertussis), a highly contagious respiratory disease.
- Haemophilus influenzae: Can cause respiratory tract infections, including pneumonia and meningitis, as well as other invasive diseases.
These are just a few examples, and there are many more Gram-negative bacteria with diverse characteristics and roles in infectious diseases and environmental processes.
What are endotoxins?
Endotoxins are toxins that are an integral part of the bacterial cell and are released when the cell disintegrates.
Endotoxemia refers to the presence of endotoxins, particularly LPS, in the bloodstream. When endotoxins enter the bloodstream, they can trigger an immune response leading to inflammation and potentially serious health consequences. Endotoxemia can result from infections caused by Gram-negative bacteria or from conditions where bacteria normally residing in the gut enter the bloodstream due to intestinal permeability issues (leaky gut syndrome).
The effects of endotoxemia on blood glucose, insulin, and triglycerides can vary depending on the individual and the severity of the endotoxemia. In general, endotoxemia can induce metabolic disturbances. Some studies suggest that acute exposure to endotoxins can lead to insulin resistance, which may result in elevated blood glucose and insulin levels. Additionally, endotoxemia has been associated with dyslipidemia, including elevated triglyceride levels. However, the specific effects may depend on factors such as the duration and severity of endotoxemia, as well as individual metabolic characteristics.
What are signs and symptoms of endotoxemia?
Endotoxemia occurs when endotoxins, such as lipopolysaccharides (LPS) from Gram-negative bacteria, enter the bloodstream and trigger an immune response. The signs and symptoms of endotoxemia can vary depending on the severity of the condition and individual factors. Some common signs and symptoms may include:
- Fever: Endotoxemia often causes an increase in body temperature as part of the immune response.
- Chills and rigors: Patients may experience sudden onset chills or rigors, which are involuntary muscle contractions often associated with fever.
- Hypotension: Endotoxemia can lead to a drop in blood pressure, potentially causing dizziness, lightheadedness, or fainting.
- Tachycardia: Increased heart rate is a common response to endotoxemia, as the body attempts to compensate for decreased blood pressure.
- Tachypnea: Rapid breathing may occur as the body tries to increase oxygen delivery to tissues.
- Malaise and weakness: Patients may feel generally unwell, fatigued, or weak.
- Gastrointestinal symptoms: Endotoxemia can cause nausea, vomiting, abdominal pain, and diarrhea.
- Headache: Some individuals may experience headaches as a result of endotoxemia.
- Altered mental status: In severe cases, endotoxemia can lead to confusion, delirium, or loss of consciousness.
- Systemic inflammatory response syndrome (SIRS): Endotoxemia may trigger a systemic inflammatory response characterized by abnormalities in body temperature, heart rate, respiratory rate, and white blood cell count.
It’s important to note that endotoxemia can progress to more severe conditions such as sepsis, septic shock, and multiple organ dysfunction syndrome (MODS) if not promptly treated. If someone experiences symptoms suggestive of endotoxemia, particularly if they have a known infection or risk factors for Gram-negative bacterial infections, they should seek medical attention immediately for proper evaluation and management.
Dr. Tom O’Bryan on STRESS, LEAKY GUT + LPS
- The stress hormones weaken and damage your gut lining, leading to leaky gut.
- Excess stress will trigger leaky gut all by itself.
- LPS breach the cell walls and floods out into your bloodstream.
- Your body senses more stress triggers more inflammation.
- You begin a never-ending cycle.
- You have an on-off switch in your body.
- You are either in “fight or flight” mode, or “rest and digest” mode.
- The body is designed to stay in the “rest and digest” mode where it functions best.
- Unfortunately, more often than not, you are in “fight or flight” mode.
- Not only is your body not in its relaxed reparation state, but it also starts to shut down systems.
- Then it enters emergency mode.
- The trick here is offering your body as much support as possible.
- This limits stress and allows it to get back to its proper restorative state.
Here are some functional lab markers that may provide clues to these conditions:
conditions:
- LPS and Endotoxins:
- LPS Binding Protein (LBP): LBP is a marker that can indicate the presence of circulating LPS in the bloodstream. Elevated levels of LBP suggest increased exposure to LPS and potential endotoxemia.
- Endotoxin Core Antibodies (EndoCAb): EndoCAb levels may reflect the immune response to LPS exposure. Lower levels of EndoCAb can indicate higher levels of circulating endotoxins.
- SIBO:
- Hydrogen and Methane Breath Test: This test measures the levels of hydrogen and methane gas produced by bacteria in the small intestine after the ingestion of a substrate (e.g., lactulose or glucose). Elevated levels of hydrogen and/or methane can indicate bacterial overgrowth in the small intestine.
- Small Intestinal Culture: Culturing a sample obtained via endoscopy can directly identify bacterial overgrowth in the small intestine.
- Small Bowel Aspirate: Aspirating fluid from the small intestine during endoscopy can be analyzed for bacterial overgrowth using various methods, including quantitative culture or PCR-based techniques.
- SIFO:
- Fungal Culture: Culture of a small intestinal aspirate or stool sample can identify the presence of fungal overgrowth in the small intestine.
- Fecal Calprotectin: Elevated levels of calprotectin in the stool can indicate intestinal inflammation, which may be associated with fungal overgrowth or other gastrointestinal conditions.
- Organic Acid Test (OAT): OAT can detect metabolites produced by fungi and bacteria in the gastrointestinal tract, providing indirect evidence of fungal overgrowth.
Additionally, comprehensive stool analysis tests (CSA) can offer insights into dysbiosis, inflammation, and other markers associated with gastrointestinal health. These tests often include assessments of microbial diversity, markers of inflammation, and levels of short-chain fatty acids (SCFAs), which can provide additional information relevant to LPS, endotoxins, SIBO, and SIFO.
It’s important to interpret these laboratory tests in the context of the patient’s clinical presentation and other diagnostic findings to guide appropriate treatment decisions. Working with a healthcare provider experienced in interpreting functional laboratory tests can help ensure accurate assessment and effective management of gastrointestinal issues.
Elevated levels of glucose, insulin, A1C (glycated hemoglobin), and triglycerides are often associated with metabolic dysfunction and conditions such as insulin resistance, type 2 diabetes, and dyslipidemia. While lipopolysaccharides (LPS) and endotoxins are primarily associated with immune responses and inflammation, there is evidence to suggest that they may also play a role in metabolic disturbances and the development of metabolic disorders.
Here’s how LPS and endotoxins may be related to these metabolic markers:
- Insulin Resistance: Chronic exposure to LPS and endotoxins has been linked to the development of insulin resistance, a condition where cells become less responsive to the effects of insulin. LPS-induced inflammation can impair insulin signaling pathways, leading to decreased glucose uptake by cells and elevated blood glucose levels. Insulin resistance is a key component of metabolic syndrome and type 2 diabetes.
- Glucose Dysregulation: LPS-induced inflammation may directly affect pancreatic beta cells, which are responsible for producing insulin. Inflammatory cytokines released in response to LPS exposure can impair beta cell function and insulin secretion, contributing to elevated blood glucose levels and impaired glucose tolerance.
- A1C: Hemoglobin A1C (HbA1c) reflects average blood glucose levels over the past 2-3 months and is used as a marker of long-term glycemic control. Chronic inflammation associated with elevated LPS and endotoxins may contribute to sustained hyperglycemia, leading to higher levels of glycated hemoglobin (HbA1c) over time.
- Triglycerides: LPS-induced inflammation can also affect lipid metabolism and contribute to dyslipidemia, characterized by elevated triglyceride levels. Inflammatory cytokines can stimulate hepatic production of triglycerides and reduce clearance of triglyceride-rich lipoproteins from the bloodstream, leading to elevated circulating triglycerides.
Overall, chronic exposure to LPS and endotoxins can contribute to metabolic dysfunction through multiple mechanisms, including inflammation-induced insulin resistance, impaired glucose regulation, and dyslipidemia.
- Addressing gut health, reducing inflammation, and improving metabolic function may help mitigate the impact of LPS and endotoxins on metabolic markers and reduce the risk of developing metabolic disorders.
- Lipopolysaccharide (LPS)-induced inflammation refers to the inflammatory response triggered by the presence of LPS, a component of the outer membrane of Gram-negative bacteria, in the body.
- When LPS enters the bloodstream, typically due to increased intestinal permeability (leaky gut) or bacterial infections, it can activate the immune system and lead to the production of pro-inflammatory cytokines and other inflammatory mediators.
- This inflammatory response plays a key role in the body’s defense against bacterial infections but can also contribute to various health problems when dysregulated.