Do you struggle with Gut Dysfunction?
Small Intestinal Bacterial Overgrowth (SIBO) is a condition where an abnormal increase in the number of bacteria occurs in the small intestine. This overgrowth can interfere with digestion, absorption, and the normal function of the gastrointestinal tract.
Signs and Symptoms of SIBO (Small Intestinal Bacterial Overgrowth):
Bile and digestive enzymes play key roles in digestion, and their relationship with SIBO is complex:
- Bile:
- Bile is produced by the liver and stored in the gallbladder, then released into the small intestine to aid in the digestion and absorption of fats. It also helps to maintain the proper balance of gut bacteria.
- In SIBO, bile production and flow can be compromised. This can be due to issues such as gallbladder dysfunction, or inadequate bile secretion, which can lead to poor digestion of fats and the development of bacterial overgrowth in the small intestine.
- Furthermore, bile has antimicrobial properties and helps control bacterial populations in the small intestine. Reduced bile flow can allow pathogenic bacteria to proliferate, contributing to or exacerbating SIBO.
- Digestive Enzymes:
- Digestive enzymes are crucial for breaking down proteins, carbohydrates, and fats into absorbable nutrients. In SIBO, impaired digestion may occur due to enzyme deficiencies or dysfunctions, often leading to malabsorption and exacerbating symptoms like bloating, gas, and diarrhea.
- The overgrowth of bacteria can also alter the pH in the small intestine, which may affect the activity of digestive enzymes. This can result in incomplete digestion, contributing to symptoms of SIBO such as discomfort and malnutrition.
Addressing SIBO with bile and digestive enzymes:
- Bile support: Some individuals with SIBO may benefit from bile salt supplements to improve fat digestion and help control bacterial overgrowth. This can also be helpful in improving bile flow and decreasing the risk of bacterial buildup.
- Digestive enzymes: Taking digestive enzymes may help those with SIBO, especially if their symptoms are related to malabsorption or insufficient enzyme activity. Enzyme supplements containing amylase, protease, and lipase can assist with breaking down carbohydrates, proteins, and fats.
However, it’s essential to approach SIBO treatment in a comprehensive and individualized manner. Consulting with a healthcare provider, such as a functional medicine practitioner, is key to determine the right approach for managing SIBO and restoring proper digestion.
Let’s dive deeper into the relationship between bile flow, digestive enzymes, and SIBO, and how to manage these factors effectively.
1. Bile Flow and SIBO
Bile is produced by the liver and stored in the gallbladder, then released into the small intestine to aid in fat digestion. It also helps maintain a healthy balance of gut bacteria by preventing the overgrowth of harmful bacteria in the small intestine. In the context of SIBO, bile flow plays several important roles:
- Antimicrobial Action: Bile has antimicrobial properties that help control bacterial populations in the small intestine. When bile flow is impaired, bacterial overgrowth can occur. This is one reason why individuals with reduced bile production or poor bile flow (due to gallbladder issues, liver dysfunction, or other factors) are more likely to develop SIBO.
- Fat Digestion: Adequate bile is needed for fat digestion. If bile flow is compromised, fat digestion becomes inefficient, which can lead to malabsorption of fat-soluble vitamins (A, D, E, K) and contribute to the feeling of bloating and discomfort that are often seen in SIBO.
- Slowed Gastric Motility: If bile flow is reduced, it can slow down the motility (movement) of the small intestine. This slower movement can allow bacteria more time to proliferate and cause overgrowth, further contributing to the SIBO cycle.
Strategies to Improve Bile Flow in SIBO:
- Bile Salts and Supplementation: If bile production is insufficient, bile salt supplements (such as ox bile) can help improve fat digestion and reduce symptoms associated with low bile production. These supplements mimic natural bile, helping the body better digest fats and control bacterial growth in the small intestine.
- Choleretics and Cholekinetics: Choleretics increase the production of bile, and cholekinetics enhance the release of bile from the gallbladder. Herbs like dandelion root, artichoke extract, and milk thistle can promote bile production and flow.
- Liver Support: Supporting the liver with nutrients like NAC (N-acetyl cysteine), taurine, or even detox protocols can help improve bile production. A healthy liver is crucial for maintaining proper bile synthesis and flow.
- Dietary Changes: High-fat meals can stimulate bile release, but if someone has compromised bile flow, eating smaller, more frequent meals might help ease the digestive process. Additionally, avoiding highly processed foods and sugars, which can exacerbate bacterial overgrowth, is essential.
2. Digestive Enzymes and SIBO
Digestive enzymes are crucial for breaking down the macronutrients (proteins, fats, and carbohydrates) in food. They play an essential role in ensuring that nutrients are absorbed in the small intestine. In individuals with SIBO, digestive enzyme deficiencies or malfunctions can exacerbate symptoms such as bloating, gas, and malabsorption.
Key Enzymes in SIBO Management:
- Protease: Breaks down proteins into amino acids. Insufficient protease activity can result in undigested protein particles, which can feed the overgrown bacteria in the small intestine, leading to more fermentation and gas production.
- Amylase: Breaks down carbohydrates into sugars. In people with SIBO, undigested carbohydrates can reach the small intestine, where they become a food source for the overgrown bacteria, worsening bloating and discomfort.
- Lipase: Breaks down fats into fatty acids and glycerol. In SIBO, if bile flow is impaired and fats are not digested properly, lipase supplementation can help digest fats more efficiently, reducing bloating and discomfort after meals.
Enzyme Supplementation for SIBO:
- Broad-Spectrum Digestive Enzymes: For many people with SIBO, a broad-spectrum digestive enzyme formula can assist in the breakdown of carbohydrates, proteins, and fats. These enzymes may help improve nutrient absorption and reduce the bloating and discomfort associated with undigested food.
- Protease and Amylase Focused Supplements: If carbohydrate and protein digestion is a major issue, supplements containing higher amounts of amylase and protease can support digestion and help reduce symptoms.
- Targeted Enzymes for SIBO-related Symptoms: In some cases, targeted enzymes may be necessary to address specific symptoms. For example, lactase enzymes might be needed for people who have difficulty digesting lactose due to bacterial overgrowth.
Enzyme Timing and Usage:
- Before Meals: Digestive enzymes are typically taken 15-30 minutes before meals to ensure that they are present when food enters the stomach. This timing helps support optimal digestion, particularly if there is a delay in gastric motility, as seen in SIBO.
- With Each Meal: Enzyme use should be consistent with every meal, especially for those who have trouble with fat digestion (often a concern in SIBO) or have malabsorption due to bacterial overgrowth.
3. Managing SIBO with Diet and Lifestyle Changes
Diet plays a critical role in managing SIBO, and when bile and enzyme production are involved, dietary choices must support healthy digestion and bacterial balance:
- Low FODMAP Diet: This diet restricts fermentable carbohydrates that are poorly absorbed in the small intestine, which are a primary fuel source for bacteria. It can help manage SIBO symptoms by reducing food for bacterial fermentation.
- SIBO-Specific Diets: These may involve specific carbohydrate restrictions (e.g., the SCD or GAPS diet) that aim to reduce bacterial overgrowth. These diets often focus on easily digestible foods that don’t exacerbate the SIBO condition.
- Small, Frequent Meals: Large meals may overwhelm the digestive system, particularly in SIBO, leading to bloating and discomfort. Smaller meals spread throughout the day can help manage symptoms.
- Avoiding Sugar and Refined Carbs: Sugar, refined carbs, and simple sugars can feed bacterial overgrowth. Maintaining a diet rich in nutrient-dense whole foods with low sugar content can help starve harmful bacteria.
- Probiotics and Prebiotics: While probiotics can be helpful in restoring balance to the gut flora, they should be used cautiously in SIBO, as some strains can actually worsen symptoms. Prebiotics (fiber) should also be monitored carefully.
Conclusion:
To manage SIBO, addressing bile flow and digestive enzyme deficiencies is crucial. This may involve:
- Supporting bile flow through bile salts and liver support.
- Using digestive enzyme supplements to improve nutrient digestion.
- Following a diet that reduces bacterial overgrowth and supports digestion.
The connection between Small Intestinal Bacterial Overgrowth (SIBO), Lactobacillus reuteri (L. reuteri), and the hormone oxytocin is an interesting area of research that explores the intricate relationship between gut health, microbiota, and hormonal regulation.
1. Lactobacillus reuteri (L. reuteri) and SIBO
L. reuteri is a probiotic bacterium commonly found in the human gut, particularly in the small intestine. It has several potential health benefits, including balancing the gut microbiota, supporting digestion, and modulating the immune system.
In the context of SIBO:
- SIBO and Dysbiosis: SIBO is often caused by an imbalance or overgrowth of bacteria in the small intestine, including both pathogenic and beneficial strains. In some cases, an overgrowth of harmful bacteria leads to dysbiosis (microbial imbalance). Conversely, beneficial bacteria like L. reuteri may play a role in restoring balance in the gut microbiome.
- L. reuteri’s Role in SIBO Management:
- Inhibition of Pathogenic Bacteria: L. reuteri has been shown to exhibit antimicrobial properties and may help outcompete or inhibit the growth of pathogenic bacteria in the small intestine, thereby potentially assisting in managing SIBO.
- Promoting Gut Barrier Integrity: L. reuteri can help improve the gut lining and overall gut health. This may reduce inflammation and help prevent the underlying factors that contribute to SIBO.
However, some caution is warranted. While L. reuteri is generally beneficial, overgrowth of any bacteria (including beneficial strains) in the small intestine can exacerbate SIBO symptoms. Therefore, introducing probiotics like L. reuteri must be approached carefully, under the guidance of a healthcare provider, especially during active SIBO.
2. L. reuteri and Oxytocin Production
Oxytocin is a hormone that plays a key role in various physiological functions, including childbirth, lactation, and emotional bonding. It is often referred to as the “love hormone” or “cuddle hormone” due to its association with social bonding, trust, and intimacy. Beyond its role in reproduction, recent research has indicated that oxytocin also has a profound influence on gut health.
L. reuteri and Oxytocin: The Connection
- Gut-Brain Axis: The gut and brain communicate bidirectionally through the gut-brain axis, a complex network that links the central nervous system (CNS) with the enteric nervous system (ENS) and gut microbiota. This connection is vital for maintaining emotional and physiological balance.
- L. reuteri and Oxytocin Regulation:
- Production of Oxytocin: Studies have shown that L. reuteri can stimulate oxytocin production. In animal models, the presence of L. reuteri in the gut microbiome has been linked to an increase in oxytocin levels in the brain. This might be due to L. reuteri’s ability to influence the central nervous system and stimulate the release of oxytocin from the hypothalamus and pituitary gland.
- Potential Benefits for Stress and Anxiety: Oxytocin has been shown to have anti-stress effects and can help regulate emotions such as anxiety, depression, and stress. By promoting the release of oxytocin, L. reuteri may contribute to improved emotional well-being, potentially lowering cortisol levels and enhancing the body’s ability to manage stress. This is significant since chronic stress is known to disrupt gut health, potentially contributing to conditions like SIBO.
- Immune System Modulation: Oxytocin also has a modulatory effect on the immune system. By promoting oxytocin production, L. reuteri may contribute to a more balanced immune response, potentially reducing inflammation in the gut and supporting the resolution of SIBO.
Oxytocin and SIBO:
Oxytocin’s role in gut motility has gained attention in recent research. As a hormone involved in smooth muscle contraction, it may help improve intestinal motility, which is crucial in SIBO management. Proper motility ensures that food and waste products move through the digestive system efficiently, reducing the likelihood of bacterial overgrowth and promoting a healthy gut environment.
Moreover, low oxytocin levels are associated with stress, which can negatively impact the digestive system, potentially exacerbating conditions like SIBO. Higher oxytocin levels, on the other hand, might help mitigate the effects of stress and improve overall gut health.
3. The Role of L. reuteri in Stress and Gut Health
The stress-gut connection is well-documented, with stress being a significant factor that can worsen SIBO and other gastrointestinal conditions. By influencing oxytocin production, L. reuteri may help reduce the impact of stress on the gut and contribute to:
- Reduced inflammation: Oxytocin has been shown to reduce the release of inflammatory cytokines, which can promote gut healing.
- Improved gut motility: Oxytocin enhances smooth muscle contractions, aiding in the proper movement of food and reducing the risk of bacterial overgrowth.
- Balancing the microbiome: A balanced gut microbiome is essential for optimal gut function and immune regulation. L. reuteri, by stimulating oxytocin, may contribute to maintaining this balance.
4. Practical Considerations in Managing SIBO with L. reuteri and Oxytocin
While the connection between L. reuteri, oxytocin, and SIBO presents an exciting area of exploration, it’s important to approach treatment with caution:
- Probiotics for SIBO: Probiotics like L. reuteri may be helpful in restoring gut health, but they should be used cautiously during active SIBO, as overgrowth of any bacteria can worsen symptoms. A low-dose introduction and gradual increase is recommended under professional guidance.
- Oxytocin Support: While L. reuteri may help stimulate oxytocin production, lifestyle factors such as social bonding, physical touch, and positive interactions can also support oxytocin levels. Managing stress through practices like meditation, yoga, or breathwork can further optimize oxytocin and support gut health.
- Gut Health and Emotional Well-being: Since the gut-brain axis is a two-way street, improving gut health with appropriate probiotics (such as L. reuteri) may not only enhance physical symptoms like bloating and discomfort but also improve emotional well-being through increased oxytocin production.
Conclusion
The connection between SIBO, Lactobacillus reuteri, and oxytocin involves a multi-faceted relationship between gut health, bacterial balance, and emotional well-being. By supporting the gut with probiotics like L. reuteri, promoting oxytocin production, and managing stress, it’s possible to improve both the physical symptoms of SIBO and emotional health. However, any treatment approach should be individualized, considering the balance between beneficial bacteria, gut motility, and hormonal regulation.
The connection between SIBO, Lactobacillus reuteri (L. reuteri), oxytocin, and food sensitivities—especially those related to histamine—is complex, as it involves interactions between the gut microbiome, the immune system, and the production of various hormones. Let’s break this down into key components:
1. SIBO and Histamine Intolerance
SIBO often leads to imbalances in the gut microbiome, which can exacerbate food sensitivities, including histamine intolerance. Histamine intolerance occurs when there is an excess of histamine in the body or an inability to break it down efficiently, often due to a deficiency in the enzymes DAO (diamine oxidase) or HNMT (histamine-N-methyltransferase), which are responsible for histamine breakdown in the gut and tissues.
In the context of SIBO:
- Bacterial Overgrowth: Many types of bacteria, including some strains of Lactobacillus and Bifidobacterium, produce histamine as a byproduct of their metabolism. When there’s an overgrowth of bacteria in the small intestine, particularly those that produce excess histamine, it can contribute to symptoms of histamine intolerance (e.g., headaches, hives, digestive distress).
- Reduced DAO Activity: SIBO may impair the function of enzymes like DAO, which are important for breaking down histamine. This leads to an accumulation of histamine in the gut and bloodstream, exacerbating inflammatory responses and food sensitivities.
2. L. reuteri and Histamine Production
Lactobacillus reuteri (L. reuteri) is a beneficial probiotic known for its ability to influence gut health in various ways, including potentially modulating histamine production.
- Histamine-Producing Properties: Some strains of L. reuteri are histamine-producing bacteria, which means that when used in excess or in individuals sensitive to histamine, it could worsen histamine intolerance. However, other strains may help to normalize histamine levels and promote balance within the microbiome.
- Supporting Gut Health: On the positive side, L. reuteri can also help improve the gut lining and the overall health of the intestinal mucosa, which may reduce inflammation and improve the digestive response to foods, potentially minimizing food sensitivities, including those related to histamine.
- Balance Is Key: Because L. reuteri can both produce and regulate histamine, it is essential to monitor how your body responds to it. In some individuals with SIBO and histamine intolerance, L. reuteri may worsen symptoms. For others, lower doses or careful management of L. reuteri may help rebalance gut flora and support better histamine breakdown.
3. Oxytocin, Stress, and Histamine Reactions
Oxytocin is involved in various aspects of gut-brain communication and can influence how the body responds to stress, which is a key trigger for food sensitivities, including histamine reactions.
- Oxytocin’s Stress-Reducing Role: As a hormone that promotes relaxation and emotional bonding, oxytocin has been shown to reduce cortisol levels, the stress hormone that can disrupt gut function and exacerbate histamine intolerance. Chronic stress is known to impair the intestinal barrier function, making the gut more prone to leaky gut and histamine-induced inflammation.
- Gut-Brain Axis: The gut-brain axis plays a major role in both food sensitivities and histamine intolerance. When oxytocin is released, it helps modulate the immune response and supports healthy gut motility. This could potentially reduce the inflammatory response that triggers histamine reactions to foods, particularly during stress.
4. Histamine Intolerance, Food Sensitivities, and SIBO
Food sensitivities, particularly histamine intolerance, are commonly observed in individuals with SIBO due to several factors:
- Imbalance of Gut Bacteria: The overgrowth of bacteria in the small intestine, especially those that produce histamine, can contribute to excess histamine in the gut. This, in turn, can lead to systemic symptoms when histamine enters the bloodstream.
- Leaky Gut: SIBO often causes inflammation and damage to the intestinal lining, increasing intestinal permeability (known as “leaky gut”). This allows histamine and other inflammatory substances to enter the bloodstream, contributing to food sensitivities and worsening histamine intolerance.
5. Connection to Food Sensitivities (including Histamine Reactions)
Food sensitivities are often immune-mediated reactions that occur when the body is exposed to foods it perceives as harmful, triggering inflammation. In the case of histamine intolerance, foods that are naturally high in histamine (e.g., fermented foods, aged cheeses, alcohol, and processed meats) can provoke symptoms like:
- Bloating
- Diarrhea
- Migraines
- Skin rashes
- Abdominal pain
The role of L. reuteri and oxytocin in modulating these sensitivities is still being explored, but:
- L. reuteri, through its influence on the microbiome, might help reduce the production of histamine-producing bacteria and support the gut’s immune function.
- Oxytocin, by lowering stress and improving gut motility, could help minimize the triggers for histamine reactions, thus improving the body’s overall ability to digest and tolerate foods.
6. Practical Implications for Managing SIBO and Histamine Intolerance
If you have both SIBO and histamine intolerance, there are several practical strategies to manage symptoms:
- Dietary Modifications: Following a low-histamine diet can help reduce symptoms. Avoiding fermented foods, aged cheeses, and alcohol (all high in histamine) may reduce reactions.
- Probiotics: While L. reuteri can be helpful in some cases, it’s important to select probiotics that don’t exacerbate histamine intolerance. Probiotics like Lactobacillus rhamnosus, Bifidobacterium longum, and Saccharomyces boulardii may be better choices for those with histamine sensitivity.
- DAO Enzyme Support: Supplementing with DAO enzymes (the enzyme responsible for breaking down histamine) can help manage histamine intolerance. It is often recommended to take DAO enzymes before meals that contain histamine-rich foods.
- Gut Healing: Focus on healing the gut lining with supplements like L-glutamine and zinc, as well as incorporating anti-inflammatory foods that can promote healing and reduce food sensitivities.
- Stress Management: Since stress can exacerbate both SIBO symptoms and histamine intolerance, managing stress through techniques like meditation, deep breathing, and oxytocin-boosting activities (like physical touch, social bonding, and positive emotions) can be helpful.
Conclusion
SIBO, histamine intolerance, L. reuteri, and oxytocin are interconnected in a complex web of gut health, immune function, and hormonal regulation. While L. reuteri may help balance gut flora and support oxytocin production, it can also exacerbate histamine reactions in certain individuals. Managing SIBO and food sensitivities requires a holistic approach that considers gut motility, stress reduction, and dietary modifications, with the goal of restoring balance to both the microbiome and the body’s immune and hormonal systems.
The relationship between SIBO (Small Intestinal Bacterial Overgrowth), poor digestion, enzymes, bile flow, gallbladder function, and poor vagal tone is quite intricate, as these factors all influence gut health, digestion, and the gut-brain connection. The vagus nerve, which is the main component of the parasympathetic nervous system, plays a central role in regulating many aspects of digestion and the overall gut microbiome. Let’s break down these connections:
1. The Role of Vagal Tone and the Vagus Nerve in Digestion
The vagus nerve is the primary component of the parasympathetic nervous system and has a key role in regulating the digestive process, including the following:
- Stimulating digestion: The vagus nerve signals the release of digestive enzymes, stomach acid, and bile, which are essential for proper food digestion and nutrient absorption.
- Regulating gut motility: It also influences the movement of food through the gastrointestinal tract by promoting peristalsis, which is the wave-like muscle contractions that move food along the digestive system.
- Balancing gut microbiota: The vagus nerve influences the composition of the gut microbiome, which in turn affects intestinal health and can help manage bacterial populations, including SIBO.
Vagal tone refers to the ability of the vagus nerve to communicate effectively and maintain a balance between the sympathetic (fight or flight) and parasympathetic (rest and digest) nervous systems. A healthy vagal tone is associated with improved digestion, immune function, and overall gut health.
When vagal tone is low or poor, the digestive process is impaired, leading to issues like slow gastric emptying, low stomach acid production, impaired bile flow, and insufficient enzyme secretion.
2. SIBO and Poor Vagal Tone
- Impaired Gut Motility: A low vagal tone can result in slowed motility in the small intestine, which leads to stagnation of food and an environment where bacteria can proliferate, contributing to the development of SIBO. If the digestive system isn’t moving food and waste through efficiently, bacteria have more time to grow and form an overgrowth in the small intestine.
- Increased Bacterial Overgrowth: Poor gut motility allows SIBO-causing bacteria to stay in the small intestine longer, creating an imbalance that further disrupts digestion and leads to symptoms like bloating, gas, and nutrient malabsorption.
- Gut-Brain Communication: The vagus nerve is a two-way street, with signals traveling from the gut to the brain and vice versa. Inadequate vagal communication can interfere with this signaling, leading to a dysregulated response to bacterial imbalances in the gut and poor gut health. This can make it harder to heal SIBO or other gut-related conditions.
3. Bile Flow and Gallbladder Function
- Vagal Nerve Influence on Bile Flow: The vagus nerve plays an essential role in the release of bile from the gallbladder. Bile is necessary for fat digestion and for helping to clear toxins from the liver and intestines. Inadequate bile flow, or cholestasis, can impair fat digestion and contribute to poor nutrient absorption.
- Impaired Bile Secretion: Low vagal tone can result in reduced bile secretion and poor gallbladder function, which disrupts the digestion of fats and the elimination of waste products. Without adequate bile flow, the digestive system can become more prone to SIBO, as the inability to break down fats properly affects overall gut health, including the environment of the small intestine.
- SIBO and Fat Malabsorption: When bile production is insufficient, fats remain undigested, leading to symptoms like steatorrhea (fatty stools) and nutrient deficiencies. This can disrupt the gut microbiome, creating an imbalance that contributes to SIBO.
4. Poor Digestion and Enzyme Function
- Pancreatic Enzymes: The vagus nerve is also responsible for signaling the release of digestive enzymes from the pancreas. Inadequate vagal tone may reduce the effectiveness of these enzymes, leading to poor digestion and malabsorption of nutrients. When digestion is impaired, food stays in the digestive tract longer, creating a favorable environment for SIBO.
- HCl (Hydrochloric Acid) Secretion: The vagus nerve triggers the secretion of HCl in the stomach, which is essential for protein digestion and for preventing the overgrowth of bacteria in the stomach and small intestine. If vagal tone is low, stomach acid production may be insufficient, contributing to the development of SIBO.
- Pancreatic and Gallbladder Dysfunction: With poor vagal tone, enzyme secretion from the pancreas may be reduced, leading to undigested food particles in the small intestine that can feed bacteria. Additionally, poor gallbladder function due to impaired vagal nerve signaling can limit the secretion of bile, which is needed to emulsify fats and support the digestive process.
5. The Gut-Brain Connection
- The vagus nerve connects the gut and brain, forming part of the gut-brain axis. When vagal tone is compromised, this communication is weakened, which can exacerbate issues like SIBO, digestive dysfunction, and even contribute to chronic stress. Chronic stress is also known to lower vagal tone, creating a vicious cycle where poor digestion and SIBO lead to more stress, which further reduces vagal function.
- Inflammation and Immune System Activation: A weakened vagus nerve connection can lead to increased inflammation and an overactive immune system, contributing to intestinal permeability (leaky gut) and an overgrowth of bacteria in the small intestine, worsening SIBO.
6. Strategies to Improve Vagal Tone and Digestive Function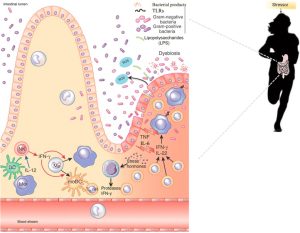
To break this cycle and improve gut health, consider the following strategies to enhance vagal tone and support digestion:
- Deep Breathing Exercises: Diaphragmatic breathing (belly breathing) activates the parasympathetic nervous system, improving vagal tone and promoting better digestion.
- Meditation and Relaxation: Practicing meditation, yoga, and other relaxation techniques can boost vagal tone and reduce chronic stress, which is a key factor in poor digestion and SIBO.
- Probiotics and Gut Healing: Supporting the gut with probiotics that promote healthy gut motility and reduce inflammation can help heal SIBO and improve overall digestive function.
- Vagus Nerve Stimulation: Techniques such as cold exposure, gargling, singing, and social bonding are all shown to stimulate the vagus nerve and improve vagal tone.
- Bile and Digestive Enzyme Support: Bile salts and digestive enzymes can support fat digestion and overall nutrient absorption, especially when bile flow is sluggish or when enzyme secretion is inadequate.
Conclusion
Low vagal tone is linked to poor digestion, bile flow, and gallbladder function, all of which contribute to the development and exacerbation of SIBO. The vagus nerve plays a critical role in regulating the release of digestive enzymes, bile, and gut motility. When vagal tone is impaired, it disrupts digestion and creates an environment where bacterial overgrowth in the small intestine can flourish. Improving vagal tone through relaxation techniques, stress management, and supporting digestive function can help improve gut health, reduce SIBO, and optimize overall digestive function.
To improve vagal tone and support SIBO and digestive health, here are some specific recommendations and approaches:
1. Techniques to Improve Vagal Tone
A. Deep Breathing and Diaphragmatic Breathing
- Deep, slow breathing activates the parasympathetic nervous system, which is linked to the vagus nerve. Practicing diaphragmatic breathing (breathing into your belly) for 5-10 minutes daily can stimulate the vagus nerve and improve digestion.
- Breathing Technique: Inhale deeply through your nose for a count of 4, hold for 4, exhale slowly through your mouth for a count of 6-8. Repeat for 5-10 minutes.
B. Meditation and Mindfulness Practices
- Mindfulness meditation, yoga, and Tai Chi can enhance vagal tone by reducing stress and stimulating the parasympathetic nervous system.
- Regular Practice: Aim for at least 10-15 minutes a day of meditation or yoga to reduce cortisol and improve gut function.
C. Cold Exposure
- Cold exposure, such as cold showers or cold plunges, has been shown to activate the vagus nerve and improve vagal tone.
- Begin Gradually: Start with cold water splashing or a cold shower for 1-2 minutes, and gradually increase the exposure over time.
D. Gargling and Singing
- Gargling with cold water, or singing loudly and deeply, can help stimulate the vagus nerve. These activities physically activate the muscles in the throat connected to the vagus nerve.
- Simple Routine: Gargle cold water for 30 seconds to 1 minute, or sing your favorite song for 5-10 minutes a few times a week.
E. Social Connection
- Engaging in social activities and positive interactions can enhance vagal tone. Studies show that positive social bonds and laughter stimulate the vagus nerve, promoting a more balanced nervous system.
2. Gut Health and SIBO-Specific Strategies
A. Addressing SIBO Directly
1. Fasting and Meal Timing
- Intermittent fasting (e.g., 12-16 hour fasts) can help reduce bacterial overgrowth by allowing the small intestine time to clear bacteria through the migrating motor complex (MMC).
- Regular Meals: Ensure you’re eating meals at consistent times to encourage gut motility and avoid prolonged periods of stagnation.
2. Low FODMAP Diet
- A Low FODMAP diet can help alleviate symptoms of SIBO by reducing the intake of fermentable carbohydrates that feed bacteria in the small intestine.
- Phases: Start with the elimination phase and gradually reintroduce foods to identify triggers.
3. Probiotics and Gut Health
- Consider specific strains of probiotics that support the gut microbiome, particularly those known for reducing small intestine bacterial overgrowth, such as Lactobacillus reuteri and Saccharomyces boulardii.
- Consultation with a practitioner: To select the right probiotic and avoid exacerbating SIBO, it’s best to consult with a healthcare professional.
4. Herbal Support
- Herbal antimicrobials like oregano oil, berberine, garlic, and berberine-containing supplements can help reduce the overgrowth of bacteria.
- Elemental Diet: A short-term elemental diet (a special liquid diet) can starve bacteria in the small intestine and reduce SIBO symptoms.
5. Digestive Enzyme and Bile Support
- Digestive enzymes can help break down food particles, making it easier for the small intestine to absorb nutrients and prevent bacterial overgrowth.
- Try enzymes that include protease, lipase, and amylase to support protein, fat, and carbohydrate digestion.
- Bile salts (e.g., ox bile) or bile support supplements can improve fat digestion and help the gallbladder release bile more effectively.
- Consider a gallbladder flush or bile-stimulating herbs (like dandelion root or milk thistle) to support bile flow if bile is sluggish.
B. Optimize Gut Motility
- Motility agents like ginger and magnesium (especially magnesium citrate) can improve gut motility, preventing food from stagnating and reducing the risk of SIBO.
- Prunes and psyllium husk (if tolerated) can also help with motility and prevent constipation, which can exacerbate SIBO.
3. Nutrient-Dense Foods for Gut Health
A. Bone Broth and Collagen
- Bone broth is rich in collagen, which can help heal the intestinal lining and support gut integrity, potentially improving digestion and vagal tone.
- Gelatin and Collagen can also support digestion and help maintain a healthy mucosal lining in the digestive tract.
B. Fiber-Rich, Easily Digestible Foods
- Low FODMAP vegetables, like zucchini, spinach, carrots, and pumpkin, are great for supporting digestion without overwhelming the gut.
- Fermented foods like sauerkraut, kimchi, and kefir (if tolerated) can support healthy gut bacteria, improve gut motility, and aid digestion.
C. Anti-Inflammatory Foods
- Omega-3-rich foods like wild-caught salmon, chia seeds, and flaxseeds can help reduce inflammation and support gut health.
- Turmeric and ginger also have anti-inflammatory properties that support digestion and improve SIBO outcomes.
4. Lifestyle Strategies
A. Stress Management
- Chronic stress can negatively impact vagal tone and digestion. Engage in stress-reducing activities such as walking, journaling, or spending time in nature to promote vagal tone and improve gut health.
- Breathwork and mindful relaxation are also excellent tools to reduce stress and support digestion.
B. Sleep Hygiene
- Aim for 7-9 hours of restorative sleep. Sleep is crucial for maintaining vagal tone, reducing stress, and promoting a balanced gut microbiome.
- Create a sleep-friendly environment by minimizing screen time before bed, maintaining a consistent sleep schedule, and optimizing room temperature for rest.
Conclusion
By improving vagal tone, addressing SIBO, enhancing digestive function, and supporting gut health, you can create a healthier digestive system and reduce symptoms like bloating, gas, and discomfort. Stress management, dietary support, and lifestyle changes are essential components to breaking the cycle of poor digestion and bacterial overgrowth.
If you’re dealing with SIBO and digestive dysfunction, it’s important to work with a healthcare provider (e.g., a functional medicine practitioner, nutritionist, or gastroenterologist) who can guide you in implementing these strategies based on your specific needs.
Dr. William Davis, a cardiologist and author of “Super Gut,” emphasizes the critical role of the gut microbiome in overall health, particularly concerning Small Intestinal Bacterial Overgrowth (SIBO), digestive enzymes, bile flow, and vagal tone.
SIBO and Gut Health
Dr. Davis identifies SIBO as a prevalent condition where harmful bacteria proliferate in the small intestine, leading to various health issues. He attributes this overgrowth to factors such as overuse of antibiotics, which disrupt the balance of beneficial gut bacteria, allowing pathogenic microbes to ascend from the colon into the small intestine. This imbalance can result in symptoms like bloating, gas, and abdominal discomfort.
Lactobacillus reuteri and Oxytocin
In “Super Gut,” Dr. Davis highlights the benefits of the probiotic strain Lactobacillus reuteri. He notes that this bacterium can stimulate the release of oxytocin, often referred to as the “love hormone.” Elevated oxytocin levels are associated with improved skin health, reduced abdominal fat, and increased muscle mass. Additionally, oxytocin contributes to emotional well-being by promoting feelings of calmness and trust.
Digestive Enzymes, Bile Flow, and Gallbladder Function
Dr. Davis discusses the importance of digestive enzymes and bile flow in maintain ing gut health. He suggests that a disrupted microbiome can impair bile production and flow, leading to digestive issues. Supporting bile flow and enzyme activity is essential for proper digestion and nutrient absorption.
ing gut health. He suggests that a disrupted microbiome can impair bile production and flow, leading to digestive issues. Supporting bile flow and enzyme activity is essential for proper digestion and nutrient absorption.
Vagal Tone and Gut Function
While Dr. Davis does not extensively cover vagal tone in his writings, he emphasizes the gut-brain connection and the impact of gut health on overall well-being. Improving gut health through dietary changes and microbiome restoration can positively influence autonomic nervous system function, including vagal tone.
Food Sensitivities and Histamine Reactions
Dr. Davis acknowledges that a disrupted microbiome can lead to food sensitivities and histamine intolerance. He notes that an imbalance in gut bacteria can impair the breakdown of histamine, leading to reactions such as headaches, hives, and digestive disturbances. Addressing SIBO and restoring a healthy microbiome can help mitigate these sensitivities.
Additional Resources
For a more in-depth understanding, Dr. Davis offers various resources:
- Website: Dr. Davis Infinite Health
- Podcast: Defiant Health Radio
- Blog: Dr. Davis Infinite Health Blog
These platforms provide valuable insights into gut health, SIBO, and related topics.

