What is PCOS and why is it so common??

In functional medicine, Polycystic Ovary Syndrome (PCOS) is often viewed as a complex, multifactorial condition influenced by various underlying imbalances rather than a single root cause.
Polycystic Ovary Syndrome (PCOS) is a common hormonal disorder that affects women of reproductive age. It is characterized by a combination of symptoms and signs, including:
- Irregular Menstrual Cycles: Women with PCOS often have infrequent, irregular, or prolonged menstrual periods. Ovulation may be absent or irregular, leading to difficulties with fertility.
- Excess Androgens: PCOS is associated with elevated levels of androgens, which are male hormones that females also produce in smaller amounts. This can lead to physical signs such as excess facial and body hair (hirsutism), acne, and thinning hair or male-pattern baldness.
- Polycystic Ovaries: The ovaries may become enlarged and contain numerous small cysts (fluid-filled sacs). Despite the name, not all women with PCOS have visible cysts on their ovaries, and the presence of cysts alone does not confirm the diagnosis.
PCOS Key Features and Causes
- Hormonal Imbalance: The hallmark of PCOS is an imbalance in reproductive hormones. This can disrupt the normal function of the ovaries, leading to issues with egg development and ovulation.
- Insulin Resistance: Many women with PCOS have insulin resistance, meaning their bodies do not use insulin effectively. This can lead to higher insulin levels, which may increase androgen production and further disrupt hormone balance.
- Inflammation: Low-grade chronic inflammation is common in PCOS, which can contribute to insulin resistance and cardiovascular risks.
- Genetics: PCOS tends to run in families, suggesting a genetic component. However, lifestyle and environmental factors also play a significant role.
PCOS Symptoms
- Irregular or absent menstrual periods
- Excess hair growth on the face and body (hirsutism)
- Acne or oily skin
- Thinning hair on the scalp

- Weight gain or difficulty losing weight
- Darkening of the skin, particularly along neck creases, groin, and underneath breasts
- Skin tags in the armpits or neck area
- Fertility issues
PCOS Complications
PCOS can lead to several long-term health issues, including:
- Infertility
- Increased risk of type 2 diabetes
- Metabolic syndrome, which includes high blood pressure, high blood sugar, abnormal cholesterol levels, and increased risk of heart disease
- Sleep apnea
- Endometrial cancer due to prolonged absence of menstruation
- Anxiety and depression
PCOS Diagnosis
PCOS is typically diagnosed based on a combination of medical history, physical examination, blood tests to measure hormone levels, and imaging tests like ultrasound to assess the ovaries.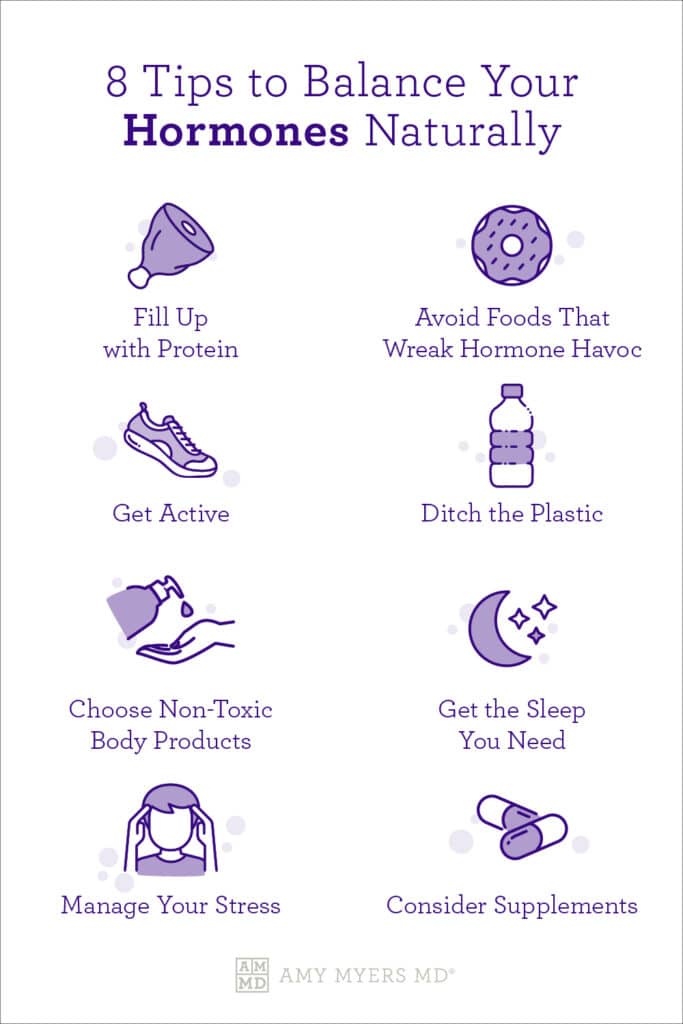
PCOS Management
Treatment of PCOS focuses on managing individual symptoms and reducing the risk of long-term complications.
Common PCOS strategies include:
- Lifestyle Changes: Diet, exercise, and weight management are first-line treatments that can improve symptoms and reduce insulin resistance.
- Medications: Hormonal birth control, anti-androgens, and medications like metformin (which improves insulin sensitivity) are commonly used.
- Fertility Treatments: For those trying to conceive, fertility medications and other interventions may be needed.
PCOS is a lifelong condition, but with proper management, many women with PCOS can lead healthy, fulfilling lives
Common contributing factors to PCOS include:
- Insulin Resistance and Blood Sugar Dysregulation: Insulin resistance is one of the most common drivers of PCOS.High insulin levels can lead to increased androgen production (such as testosterone), which disrupts normal ovarian function and contributes to symptoms like irregular periods, ovarian cysts, and hirsutism.
- Hormonal Imbalances: Imbalances in hormones, including elevated androgens (male hormones), estrogen dominance, and low levels of progesterone, are commonly seen in PCOS.
- These hormonal imbalances can lead to irregular menstrual cycles, ovulatory dysfunction, and other symptoms associated with PCOS.
- Chronic Inflammation: Low-grade chronic inflammation is another common underlying factor in PCOS.
- Inflammation can exacerbate insulin resistance and contribute to hormonal imbalances.
- It may be driven by factors such as poor diet, gut dysbiosis, environmental toxins, and stress.
- Adrenal Dysfunction: In some women with PCOS, the adrenal glands produce excess androgens, contributing to the condition.
- Stress and adrenal dysfunction, including high levels of cortisol, can exacerbate the symptoms of PCOS.
- Gut Health Issues: Gut dysbiosis and poor gut health can influence systemic inflammation, insulin sensitivity, and hormone regulation, all of which are implicated in PCOS.
- Addressing gut health through diet, probiotics, and lifestyle changes can be an essential aspect of managing PCOS in functional medicine.
- Nutrient Deficiencies: Deficiencies in key nutrients, such as magnesium, vitamin D, B vitamins, and omega-3 fatty acids, can affect hormone balance, insulin sensitivity, and inflammation, contributing to the development and persistence of PCOS.
- Environmental Toxins and Endocrine Disruptors: Exposure to environmental toxins and endocrine-disrupting chemicals (like BPA, phthalates, and pesticides) can impact hormone regulation and contribute to the development of PCOS.
- Functional medicine often emphasizes reducing exposure to these toxins as part of a comprehensive management plan.
- Genetics and Epigenetics: While genetics can play a role in PCOS, functional medicine also considers epigenetic factors—how lifestyle, diet, and environment can influence gene expression and contribute to the condition.

In functional medicine, the approach to managing PCOS involves identifying and addressing these root causes through personalized interventions, including dietary changes, targeted supplementation, lifestyle modifications, stress management, and other integrative therapies aimed at restoring balance and optimizing overall health.
In functional medicine, identifying and addressing the root causes of PCOS involves a comprehensive approach that includes functional lab testing to gain deeper insights into hormonal imbalances, metabolic dysfunction, and other underlying factors.
Here are some key functional lab tests that are commonly recommended for evaluating PCOS and exploring its root causes:
Functional Lab Tests for PCOS
- Comprehensive Hormone Panel:
- Testosterone (Total and Free): Elevated levels of testosterone are common in PCOS.
- DHEA-S (Dehydroepiandrosterone Sulfate): High levels can indicate adrenal involvement in androgen production.
- Estradiol: To assess estrogen levels and check for estrogen dominance.
- Progesterone: To evaluate ovulation and luteal phase function.
- LH (Luteinizing Hormone) and FSH (Follicle-Stimulating Hormone): A higher LH to FSH ratio (usually above 2:1) is often seen in PCOS.
- SHBG (Sex Hormone-Binding Globulin): Low levels can indicate high free testosterone, common in PCOS.
- Anti-Müllerian Hormone (AMH): Often elevated in PCOS, indicating increased ovarian reserve or dysfunction.
- Insulin and Blood Sugar Testing:
- Fasting Insulin: To detect insulin resistance, which is a common driver of PCOS.
- HOMA-IR (Homeostatic Model Assessment of Insulin Resistance): To assess insulin resistance.
- HbA1c: To evaluate average blood sugar levels over the past three months.
- Fasting Glucose: Baseline blood sugar levels.
- Comprehensive Thyroid Panel:
- TSH (Thyroid-Stimulating Hormone), Free T4, Free T3, Reverse T3, and Thyroid Antibodies (TPO and TgAb): Thyroid dysfunction can mimic or exacerbate PCOS symptoms.
- Cortisol and Adrenal Testing:

- Salivary or DUTCH Test: To assess cortisol levels throughout the day, as stress and adrenal dysfunction can contribute to PCOS.
- Lipid Panel:
- To evaluate cholesterol levels, as women with PCOS often have dyslipidemia, which increases cardiovascular risk.
- Vitamin and Mineral Deficiencies:
- Vitamin D: Often low in women with PCOS, and sufficient levels are crucial for insulin sensitivity and reproductive health.
- Magnesium, B12, Folate, and Iron: Important for overall metabolic function and hormone balance.
- Inflammation Markers:
- CRP (C-Reactive Protein) and ESR (Erythrocyte Sedimentation Rate): To evaluate systemic inflammation, which is common in PCOS.
- Gut Health Tests:
- Comprehensive Stool Analysis: To assess gut dysbiosis, which can contribute to inflammation, insulin resistance, and hormonal imbalances.
- SIBO Breath Test: Small Intestinal Bacterial Overgrowth can be an underlying factor in gut-related issues.
Root Causes of PCOS in Functional Medicine
- Insulin Resistance: A primary driver of PCOS, leading to increased androgen production, disrupted ovarian function, and weight gain.
- Hormonal Imbalances: Elevated androgens, low progesterone, and altered estrogen levels contribute to the symptoms of PCOS.
- Chronic Inflammation: Persistent low-grade inflammation can exacerbate insulin resistance and hormone dysregulation.
- Adrenal Dysfunction: Excess stress and abnormal cortisol levels can lead to increased production of adrenal androgens, contributing to PCOS symptoms.
- Nutrient Deficiencies: Deficiencies in key nutrients such as vitamin D, magnesium, and omega-3 fatty acids can impair insulin sensitivity and hormone regulation.
- Gut Dysbiosis: Imbalances in gut bacteria can contribute to systemic inflammation and metabolic dysfunction, affecting PCOS.
- Environmental Toxins: Exposure to endocrine-disrupting chemicals (EDCs) like BPA, phthalates, and pesticides can interfere with hormone balance.
- Genetic and Epigenetic Factors: While genetics can predispose individuals to PCOS, lifestyle, diet, and environmental factors play a significant role in its expression and severity.
Addressing these root causes through a personalized, functional approach—focusing on diet, lifestyle, targeted supplementation, and reducing toxin exposure—can help manage PCOS symptoms and improve overall health outcomes.
Contact Coach Debbie Potts to learn more how to improve the WHOLE you!
More PCOS Resources:
- https://www.thewomensdietitian.com/
- https://www.larabriden.com/4-types-of-pcos-a-flowchart/
- https://www.amymyersmd.com/article/pcos
- https://drchristinemaren.com/functional-medicine-approach-pcos/
- https://www.drhagmeyer.com/pcos-taking-a-functional-medicine-approach/
