Are we not eating enough (LEA)… or not eating enough carbohydrates (LCA)?
What is too low of carbohydrate intake? LCA can cause hormone imbalances in peri- and post-menopausal women, even if they are metabolically healthy, fat-adapted, and efficient at burning fat. This happens because carbohydrates play a critical role in hormonal regulation, particularly for women, whose hormonal systems are more sensitive to energy and nutrient availability.
1. Impact on Kisspeptin and Sex Hormones
Carbohydrates are crucial for the production of kisspeptin, a neuropeptide that regulates reproductive hormones such as estrogen, progesterone, and luteinizing hormone (LH). A significant reduction in carbohydrate intake can signal to the brain that the body is in an energy-deficient state, which can lead to disrupted kisspeptin activity. For peri- and post-menopausal women who are already experiencing fluctuating hormone levels, this can exacerbate imbalances and lead to issues like:
- Irregular or absent menstrual cycles (in perimenopausal women)
- Lower estrogen levels, which may cause symptoms like hot flashes, mood changes, and increased risk of bone density loss
- Reduced sensitivity to insulin, even in metabolically flexible individuals, causing impaired glucose tolerance
2. Cortisol and Stress Response
In metabolically healthy and fat-adapted women, chronic low carbohydrate intake can still lead to elevated cortisol levels. When carbohydrates are insufficient, the body perceives it as a form of stress and increases cortisol production to mobilize stored glucose (via gluconeogenesis). Elevated cortisol levels over time can result in:
- Increased abdominal fat storage
- Thyroid dysfunction (lower T3 levels), slowing metabolism and affecting energy levels
- Impaired ability to burn fat effectively, as chronic stress shifts the body toward glucose dependence, undermining metabolic flexibility
3. Thyroid Health
Even in fat-adapted women, an overly low-carbohydrate diet can negatively impact thyroid function. Thyroid hormones (particularly T3) are essential for metabolic regulation, and their production is sensitive to energy availability, particularly carbohydrates. Low-carb diets can lead to:
- Lower T3 production: This reduces metabolic rate and may cause fatigue, weight gain, and cold intolerance, despite being metabolically efficient.
- Thyroid downregulation: Over time, the lack of carbs can signal the body to conserve energy, leading to a slower metabolism and reduced fat-burning capacity.
4. Metabolically Flexible and Fat-Adaptive Individuals
For those who are metabolically healthy and fat-adapted, the body is generally efficient at switching between burning carbohydrates and fat for fuel. However, peri- and post-menopausal women still require a balance of nutrients to maintain hormonal homeostasis. Being fat-adapted doesn’t completely eliminate the need for carbohydrates in the context of hormonal balance:
- Carbohydrate timing: Strategically incorporating carbohydrates around workouts or in the evening may help maintain cortisol balance and improve sleep quality, which is often disrupted during menopause.
- Insulin sensitivity: While fat-adapted women may maintain good insulin sensitivity, carbohydrate intake supports leptin and ghrelin regulation, which can prevent cravings, mood swings, and energy crashes.
5. Energy Availability and Reproductive Health
For women in peri- and post-menopause, energy availability becomes a crucial factor. Even in a metabolically flexible individual, very low carbohydrate intake can signal to the body that there isn’t enough energy available to sustain reproductive functions. This can result in:
- Reduced production of sex hormones, exacerbating the already declining levels of estrogen and progesterone during menopause
- Increased stress response, leading to further hormone imbalances and metabolic disruption
6. Bone Health and Estrogen
Estrogen plays a critical role in maintaining bone density. For women in post-menopause, estrogen levels naturally drop, increasing the risk of osteoporosis. Too low of a carbohydrate intake can further reduce estrogen production, accelerating bone density loss. While a fat-adapted state may be metabolically healthy, it does not fully protect against the hormonal shifts related to low estrogen and low energy availability.
Here’s a concise explanation and bullet list summarizing the key points from Dr. James’s message regarding carbohydrate intake:
Recommended Carbohydrate Intake
- Minimum Intake: Nearly everyone should consume at least 40 grams of carbohydrates per day.
- Brain and Red Blood Cells: The brain requires about 130 grams of glucose daily.
- Alternative Glucose Production:
- Dietary Fat: Can provide about 8 grams of glucose.
- Fat Burning: Contributes approximately 26 grams of glucose.
- Ketone Production: Accounts for around 58.5 grams of glucose.
- Total Glucose Production: Up to 92.5 grams can be produced from fat and ketones, requiring an additional 37.5 grams of glucose from protein.
- Protein Efficiency: Protein is only 50% effective in converting to glucose, necessitating 75 grams of protein to meet glucose needs when carbohydrates are low.
- Spare Protein: Eating 40 grams of carbohydrates can help spare the need for 75 grams of protein for gluconeogenesis.
Hormonal Considerations
- Consuming 50 grams of carbohydrates daily may prevent drops in active thyroid hormone T3.
- Very low-carb diets can increase levels of cortisol and adrenaline, mimicking starvation, which is not optimal for health and longevity.
Optimal Carbohydrate Range
- General Population: 40 to 150 grams of carbohydrates per day is likely optimal.
- Athletes: May require 300+ grams of carbohydrates daily.
Carbohydrate Sources
- Optimal Sources:
- Grass-fed dairy
- Organic potatoes, sweet potatoes, and purple potatoes
- Organic fruits (e.g., strawberries, blueberries, nectarines, mangos, peaches)
- Avocados
- Raw honey and maple syrup
- Sources to Limit:
- Rice (high glycemic index, minimal nutrients)
- 100% whole grains (often highly refined, can contain glyphosate)
- Sources to Avoid:
- Ultra-processed carbohydrates (e.g., breads, pastries, muffins)
Summary
- Carbohydrates are essential for energy, hormone balance, and optimal health.
- A balanced intake of carbohydrates can enhance workout performance and overall well-being.
This summary encapsulates Dr. James’s perspective on carbohydrate consumption and its implications for health and performance.
Here are examples of gluten-free, grain-free, easy-to-digest pre-workout snacks that provide about 10 grams of carbohydrates:
- Half a Banana
- Carbs: ~10-12 grams
- A classic option that is easy to digest and rich in potassium, which supports muscle function.
- Small Apple (about 2 inches in diameter)
- Carbs: ~10 grams
- Provides a quick source of simple carbohydrates without grains or gluten.
- Dates (1 to 2 pieces)
- Carbs: ~10 grams for 1-2 small dates
- Dates are rich in natural sugars and easy on the stomach.
- Coconut Water (6-8 oz)
- Carbs: ~9-11 grams
- Hydrates while providing simple sugars for energy, ideal for pre-workout.
- Homemade Energy Balls (Made from Coconut Flour & Almond Butter)
- Carbs: ~10 grams per ball
- You can make a simple energy ball using coconut flour, almond butter, and a touch of honey or dates to hit the 10g carb mark.
- Sweet Potato (2 oz)
- Carbs: ~10 grams
- Cooked sweet potatoes are naturally gluten-free and provide a gentle source of carbs and fiber.
- Chia Pudding (2 tbsp chia seeds, ½ cup coconut milk)
- Carbs: ~10 grams
- Mixed with a small amount of honey or maple syrup, chia pudding can provide both carbs and healthy fats for sustained energy.
- Small Handful of Dried Mango (1 oz)
- Carbs: ~10 grams
- Dried fruit provides concentrated carbs in a small serving, making it easy to digest and consume pre-workout.
These options are all gluten and grain-free while offering a quick, digestible source of carbohydrates to fuel your workout without causing digestive discomfort.
Key Considerations for Carbohydrate Intake:
- Personalized Approach: Carbohydrate needs are individual and should be adjusted based on activity levels, stress, and overall health. While fat-adapted athletes may thrive on lower carbs, peri- and post-menopausal women still need some carbohydrates to support hormonal health.
- Targeted Carbohydrate Consumption: Focus on nutrient-dense, low-glycemic carbohydrates like vegetables, fruits, and whole grains to support hormonal balance without causing blood sugar spikes.
- Carb Cycling: Women in this age group can benefit from carb cycling, where carbs are increased on active days or around intense workouts to ensure adequate energy and hormone regulation.
Even metabolically healthy and fat-adapted peri- and post-menopausal women need some carbohydrate intake to avoid hormone imbalances.
- Severe carbohydrate restriction can disrupt the production of kisspeptin, increase cortisol levels, and impair thyroid function, leading to further hormonal dysregulation.
- Balancing carb intake with fat adaptation, and considering individual hormonal needs and lifestyle factors, is essential for long-term health and performance.
- Intermittent fasting and keto can disrupt kisspeptin production, a key hormone involved in appetite regulation and insulin sensitivity.
- When the brain senses a deficiency in nutrients, particularly carbohydrates, kisspeptin levels drop, which increases appetite and decreases insulin sensitivity.
- This is why intermittent fasting can lead to glucose intolerance in women but not men.
- Adding exercise stress to the mix further elevates cortisol levels, keeping the body in a heightened sympathetic state, reducing the ability to relax, and impairing thyroid function.
- This can lead to disrupted menstrual cycles, increased belly fat storage, heightened anxiety, and impaired athletic performance, often resulting in weight gain—counteracting the desired outcomes of fasting.
Source: Dr. Stacy Sims’ blog.
“As I’ve said many times, from a health standpoint, intermittent fasting is useful. This is particularly true for the general population who are not very active and struggling with metabolic diseases. However, when you dig deeper and look at longevity data in terms of both intermittent fasting and exercise, they’re both beneficial, but you do not garner any additional benefits from layering intermittent fasting on top of exercising (which I know you all do!)” https://www.drstacysims.com/blog/You_are_an_athlete_and_you_shouldn%E2%80%99t_practice_intermittent_fasting
References in Dr. Sims blogs include:
- https://link.springer.com/article/10.1007/s40279-018-0867-7
- https://www.mdpi.com/2072-6643/15/20/4457#B20-nutrients-15-04457
- https://www.frontiersin.org/journals/endocrinology/articles/10.3389/fendo.2018.00123/full
- https://www.nature.com/articles/s41574-020-0363-7
Kisspeptin’s Role in Fat Metabolism and Insulin Sensitivity:
Kisspeptin is a neuropeptide that plays a critical role in regulating sex hormones and reproductive health, but its influence extends to metabolic processes, such as fat metabolism and insulin sensitivity.
1. Fat Metabolism:
- Energy Availability: Kisspeptin neurons respond to the body’s energy state, such as the availability of fat and glucose. When energy levels are adequate, kisspeptin signaling supports normal metabolic function, including efficient fat metabolism.
- Fat Storage: Disruptions in kisspeptin signaling, caused by stress, nutrient deprivation, or low energy intake, can impair the body’s ability to metabolize fat. This can lead to changes in how fat is stored and used, potentially contributing to increased fat storage or difficulty burning fat.
- Appetite and Energy Expenditure: Kisspeptin may also influence energy expenditure rather than directly controlling food intake, affecting how the body burns energy, including fats, during physical activity or rest.
2. Insulin Sensitivity:
- Glucose Control: Kisspeptin has a significant role in glucose metabolism and insulin sensitivity. By influencing how the body uses glucose, kisspeptin helps maintain balanced blood sugar levels.
- Stress and Energy Deficits: When kisspeptin signaling is disrupted, insulin sensitivity can decrease, making it harder for the body to use glucose effectively. This can result in higher blood sugar levels and a risk of insulin resistance, which is often seen in metabolic disorders like type 2 diabetes.
- Hormonal Impact: Since kisspeptin regulates sex hormones like estrogen and testosterone, and these hormones are linked to insulin sensitivity, any disruption in kisspeptin can also indirectly affect how sensitive the body is to insulin.
In summary, kisspeptin plays a key role in maintaining fat metabolism and insulin sensitivity, both of which are crucial for overall metabolic health. Disruptions to kisspeptin signaling—often triggered by stress, poor nutrition, or energy deficits—can lead to metabolic imbalances, affecting how the body stores fat and controls blood sugar. This makes kisspeptin particularly important for women, whose hormonal and metabolic systems are more sensitive to changes in kisspeptin levels.
The mechanism of action behind the effects of intermittent fasting (IF) and keto on women’s bodies, particularly on kisspeptin, involves several key physiological processes:
1. Kisspeptin Regulation and Nutrient Deficiency
- Kisspeptin is a hormone that plays a crucial role in regulating reproductive hormones and metabolic functions.
- It is sensitive to energy and nutrient availability, especially carbohydrates.
- When your brain perceives a lack of key nutrients (e.g., during keto or fasting), it reduces kisspeptin production.
- This downregulation occurs because the body interprets the absence of carbohydrates as a sign of scarcity, triggering a stress response.
2. Impact on Insulin Sensitivity
- Kisspeptin and Insulin Sensitivity: Kisspeptin helps maintain insulin sensitivity, a process crucial for regulating blood glucose levels.
- Lower kisspeptin leads to reduced insulin sensitivity, which can result in impaired glucose tolerance, particularly in women.
- This is more pronounced because women’s metabolic and hormonal systems are more sensitive to energy deficits.
3. Stress Response and Cortisol
- Cortisol Increase: Fasting, especially when combined with exercise, elevates the production of cortisol, a stress hormone.
- Cortisol is already naturally higher during fasting since the body is trying to mobilize stored energy.
- Adding the physical stress of exercise to an already fasting state amplifies this response.
- Sympathetic Nervous System Activation: The constant increase in cortisol keeps the body in a sympathetic (fight-or-flight) state.
- This not only makes it harder to relax but also signals the body to conserve energy and shift into fat storage mode, especially in the abdominal region.
4. Thyroid Suppression
- Thyroid Hormone Reduction: Prolonged fasting and energy deficits, especially in women, can lower thyroid hormone levels (T3 and T4).
- This is part of the body’s natural response to conserve energy.
- When thyroid activity is depressed, metabolic rate decreases, making it harder to burn fat and maintain regular menstrual cycles.
5. Menstrual Cycle Disruption
- Impact on Reproductive Hormones: Reduced kisspeptin affects the hypothalamic-pituitary-gonadal (HPG) axis, which regulates reproductive hormones like estrogen and progesterone.
- The brain essentially deprioritizes reproduction when it perceives an energy deficit, disrupting normal menstrual function, leading to irregular periods or amenorrhea.
6. Weight Gain and Fat Storage
- Fat Storage: As cortisol levels rise and kisspeptin falls, the body becomes more prone to storing fat, especially in the belly, due to the heightened stress state.
- At the same time, reduced insulin sensitivity leads to inefficient glucose utilization, promoting fat storage rather than fat burning.
In summary, fasting or keto triggers a nutrient-sensing mechanism that lowers kisspeptin production, increasing stress hormones and impairing glucose metabolism.
In women, this combination leads to metabolic, hormonal, and performance challenges, such as impaired glucose tolerance, increased fat storage, menstrual cycle disruptions, and heightened stress.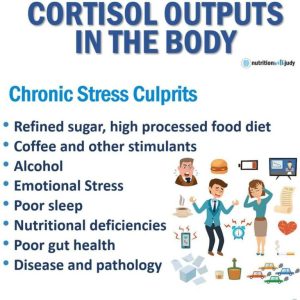
The mechanism of action for how chronic high-intensity exercise can elevate cortisol and promote fat storage, particularly around the abdomen, involves several key physiological processes:
1. Cortisol and Stress Response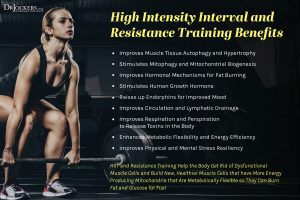
- Cortisol is the body’s primary stress hormone, released by the adrenal glands in response to physical and psychological stress. In the context of high-intensity exercise, cortisol is naturally elevated to mobilize energy (glucose and fat) to fuel the activity.
- Chronic high-intensity exercise without adequate recovery leads to sustained cortisol elevation.
- While cortisol helps mobilize stored energy during short-term stress or exercise, chronically elevated cortisol begins to have detrimental effects.
2. Impact on Fat Storage
- Fat storage in the abdomen: Chronically elevated cortisol increases fat storage, especially in the visceral or abdominal area.
- This happens because cortisol triggers the release of fatty acids into the bloodstream from fat stores, but when the body is repeatedly exposed to high cortisol levels, it starts storing more fat—particularly in the abdomen, where fat cells have a higher density of cortisol receptors.
- Glucose and fat metabolism: In the presence of high cortisol, the body becomes more reliant on glucose as its primary fuel source rather than fat. This means that instead of efficiently burning fat for fuel, the body favors glucose utilization, leaving fat stores intact or increasing them over time.
- Chronic stress reduces the body’s ability to metabolize fat effectively.
3. Insulin Resistance and Belly Fat
- Insulin sensitivity decreases with prolonged cortisol elevation. High cortisol levels make the body more resistant to insulin, leading to higher circulating glucose levels and promoting fat storage rather than fat burning.
- Abdominal fat cells are particularly sensitive to insulin and cortisol, which makes the abdominal area more prone to storing excess fat during times of prolonged stress and elevated cortisol.
4. Sympathetic Dominance and Recovery Deficit
- Sympathetic nervous system activation: Intense exercise places the body in a sympathetic state (fight-or-flight mode), with high cortisol levels sustaining this state. Over time, without proper recovery, the parasympathetic nervous system (rest-and-digest system) is not adequately engaged, leading to sympathetic dominance. This impairs recovery, reduces the body’s ability to repair tissues, and maintains high cortisol levels, perpetuating the cycle of fat storage.
5. Impaired Fat Metabolism
- Cortisol’s effect on fat metabolism: In normal circumstances, cortisol helps mobilize fat from fat stores to be used as fuel during exercise. However, chronic cortisol elevation shifts the body toward a glucose-reliant metabolism, reducing the efficiency of fat utilization. When cortisol is high for long periods, the body prioritizes glucose to handle stress, and fat oxidation (fat burning) becomes less effective.
6. Recommendation for Balance and Recovery
- Adequate recovery: Dr. Stacy Sims emphasizes the need to balance high-intensity exercise with proper recovery periods to avoid chronic cortisol elevation. Recovery allows the parasympathetic nervous system to take over, lowering cortisol levels, and shifting the body toward more efficient fat metabolism.
- Fat metabolism and stress management: Sims recommends incorporating stress management strategies (like meditation, restorative activities, and sleep) to regulate cortisol. When cortisol is managed effectively, the body is more likely to rely on fat as a fuel source during both exercise and rest, promoting healthier fat distribution and preventing excess fat storage in the abdomen.
Chronic high-intensity exercise leads to sustained elevations in cortisol, which shifts the body away from efficient fat metabolism toward glucose dependence. High cortisol levels also promote fat storage, particularly in the abdominal region, by increasing insulin resistance and reducing the body’s ability to burn fat. Balancing exercise with adequate recovery and stress management helps lower cortisol levels, improve fat oxidation, and prevent unwanted fat accumulation.
Mechanism of Action for Kisspeptin and Insulin Sensitivity:
Kisspeptin, primarily known for its role in regulating the reproductive axis, also plays a critical role in maintaining insulin sensitivity—the body’s ability to respond effectively to insulin and regulate blood glucose levels.
The following outlines how kisspeptin influences insulin sensitivity and why this process is particularly relevant for women:
1. Kisspeptin’s Interaction with the Hypothalamus and Peripheral Tissues
- Hypothalamus as a Central Regulator: Kisspeptin neurons, located in the hypothalamus, are key regulators of several endocrine and metabolic processes, including insulin sensitivity. The hypothalamus integrates signals related to energy availability, such as nutrient levels, and adjusts the body’s response to ensure proper energy homeostasis.
- Metabolic Coordination: Kisspeptin’s activity influences multiple organs through the neuroendocrine system. Beyond its reproductive function, kisspeptin affects peripheral tissues such as the liver, muscles, and adipose (fat) tissue—key players in glucose metabolism and insulin sensitivity.
- In conditions of normal kisspeptin signaling, these tissues respond efficiently to insulin, allowing glucose to be taken up from the bloodstream and used for energy or stored for later use. This process maintains healthy blood glucose levels and insulin sensitivity.
2. Impact of Reduced Kisspeptin on Insulin Sensitivity
- Decreased Insulin Sensitivity: When kisspeptin levels are reduced (due to factors like stress, fasting, or energy deficits), there is a corresponding decrease in insulin sensitivity. This means that cells in the body become less responsive to insulin, leading to higher levels of circulating glucose (blood sugar). Over time, this reduced sensitivity can lead to impaired glucose tolerance or insulin resistance, where the body needs to produce more insulin to manage blood glucose levels.
- Impaired Glucose Tolerance: As kisspeptin levels drop, the body struggles to manage glucose effectively. This impaired tolerance results in higher blood sugar levels after eating and a slower return to normal levels. Over time, chronic reductions in kisspeptin can increase the risk of developing conditions like type 2 diabetes.
3. Why Women Are More Affected by Reduced Kisspeptin Levels
- Greater Sensitivity to Energy Deficits: Women’s metabolic and hormonal systems are more sensitive to energy availability, meaning that even mild caloric deficits or stressors can disrupt kisspeptin production. Because of this heightened sensitivity, women are more prone to metabolic changes when kisspeptin signaling is disrupted.
- For example, periods of fasting, extreme calorie restriction, or excessive exercise can quickly reduce kisspeptin levels, leading to hormonal and metabolic disturbances, including reduced insulin sensitivity.
- Sex Hormone Fluctuations and Metabolism: Kisspeptin is tightly linked to the regulation of sex hormones like estrogen and progesterone, which also influence insulin sensitivity. In women, particularly during times of hormonal fluctuation (e.g., the menstrual cycle, pregnancy, or menopause), insulin sensitivity naturally fluctuates.
- When kisspeptin levels drop, it not only disrupts reproductive hormone production but also leads to reduced insulin sensitivity, compounding the effects of hormonal shifts. This can result in worse glucose tolerance during certain phases of the menstrual cycle or during menopause, where insulin sensitivity typically declines.
4. Energy Deficit and Sympathetic Nervous System Activation
- Stress Response: When the body experiences an energy deficit (whether from poor nutrition or excessive exercise), stress hormones like cortisol rise. This activates the sympathetic nervous system, increasing the body’s reliance on glucose as a quick energy source. However, reduced kisspeptin levels in these scenarios impair insulin’s ability to facilitate glucose uptake, worsening glucose control.
- Effect on Adipose Tissue: In addition, reduced kisspeptin affects fat storage, particularly in the abdominal region, where insulin resistance is more likely to occur. The body starts storing more fat, especially in response to the increased cortisol and stress associated with impaired kisspeptin signaling, further decreasing insulin sensitivity and metabolic flexibility.
5. Long-term Implications of Reduced Kisspeptin and Insulin Sensitivity
- Chronic Metabolic Disruption: Prolonged reductions in kisspeptin levels can lead to chronic insulin resistance, increasing the risk of developing metabolic disorders such as type 2 diabetes and cardiovascular diseases. In women, who are more vulnerable to these changes, the effects can be even more pronounced.
- Reproductive and Metabolic Health Link: Reduced kisspeptin levels not only impair insulin sensitivity but also disrupt reproductive hormone balance. In conditions like polycystic ovary syndrome (PCOS), a common reproductive and metabolic disorder, both insulin resistance and hormonal imbalances are present, potentially linking these conditions to impaired kisspeptin signaling.
Summary of Mechanism of Action:
- Kisspeptin helps maintain insulin sensitivity by ensuring proper communication between the hypothalamus, endocrine system, and peripheral tissues like muscles, liver, and fat.
- When kisspeptin levels are reduced (due to energy deficits, fasting, or stress), insulin sensitivity declines, leading to impaired glucose tolerance.
- Women are more sensitive to changes in kisspeptin due to their reproductive hormones and energy-sensitive metabolic systems, making them more vulnerable to reduced insulin sensitivity in response to metabolic stress.
- Chronic reductions in kisspeptin can lead to long-term metabolic issues, including insulin resistance, increased fat storage, and higher risk of metabolic diseases, particularly in women.


