What is SIBO?
SIBO stands for Small Intestinal Bacterial Overgrowth, and SIFO stands for Small Intestinal Fungal Overgrowth. Dr. William Davis, in his book “SUPER GUT,” likely discusses these conditions in the context of gut health and microbiome balance.
SIBO occurs when there’s an overgrowth of bacteria in the small intestine, which can lead to various digestive issues like bloating, gas, diarrhea, and abdominal pain. On the other hand, SIFO involves an overgrowth of fungi, particularly Candida species, in the small intestine.
Dr. William Davis may propose a protocol within “SUPER GUT” to address these conditions. His protocol might involve dietary changes, such as eliminating certain carbohydrates that feed bacteria and fungi, along with antimicrobial treatments to reduce the overgrowth. Probiotics and other gut-supporting supplements may also be recommended to restore balance to the microbiome.
The goal of the “SUPER GUT” protocol, as with many approaches to SIBO and SIFO, is to rebalance the gut microbiome, reduce symptoms, and improve overall digestive health. By addressing the underlying causes of overgrowth and supporting the growth of beneficial bacteria, individuals may experience relief from their symptoms and improved gut function.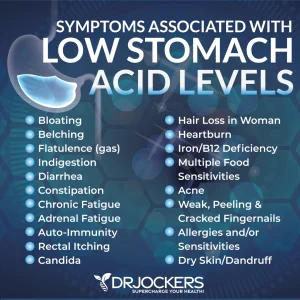
FODMAPs are a group of fermentable carbohydrates that can trigger digestive symptoms in some people, especially those with irritable bowel syndrome (IBS) or other gastrointestinal issues.
High FODMAP foods include:
- Fruits: Apples, pears, mangoes, watermelons, cherries, peaches, and canned fruit in natural fruit juice.
- Vegetables: Garlic, onions, asparagus, cauliflower, mushrooms, sugar snap peas, and snow peas.
- Legumes: Beans, lentils, chickpeas, and soybeans.
- Dairy: Milk, yogurt, and soft cheeses like ricotta and cottage cheese.
- Wheat: Bread, pasta, cereals, and other products containing wheat.
- Sweeteners: Honey, agave syrup, high-fructose corn syrup, and foods with artificial sweeteners containing sorbitol, mannitol, xylitol, and maltitol.
It’s important to note that not all of these foods will affect everyone in the same way. Some people may be able to tolerate small amounts, while others may need to avoid them altogether. A low FODMAP diet, typically followed under the guidance of a healthcare professional, involves temporarily restricting high FODMAP foods and then reintroducing them to identify personal triggers.
If you suspect you might be reactive to FODMAPs, there are several signs and symptoms to look out for.
These may include:
- Digestive Issues: Symptoms such as bloating, gas, abdominal pain, diarrhea, or constipation after consuming certain foods.
- Changes in Bowel Habits: Alternating between diarrhea and constipation, or experiencing frequent urgency to use the restroom.
- Abdominal Discomfort: General discomfort or pain in the abdominal region that is relieved after a bowel movement.
- Bloating: Feeling excessively full or bloated, especially after meals.
- Nausea: Feeling queasy or nauseous after eating certain foods.
- Fatigue: Feeling tired or lethargic, possibly due to nutrient malabsorption caused by gastrointestinal issues.
If you experience these symptoms regularly, it might be worth considering whether a FODMAP intolerance could be contributing to your discomfort. Keep a food diary to track your symptoms and identify any patterns related to your diet.
To confirm whether you have a sensitivity to FODMAPs, it’s best to consult with a healthcare professional, such as a gastroenterologist or a registered dietitian. They can help you undergo proper testing, such as a hydrogen breath test, and guide you through an elimination diet followed by a reintroduction phase to identify specific triggers. Additionally, they can provide personalized dietary advice and support to manage your symptoms effectively.
What are FODMAPS?
FODMAPs, an acronym for Fermentable Oligosaccharides, Disaccharides, Monosaccharides, and Polyols, are types of carbohydrates found in various foods.
These carbohydrates are fermentable, meaning they can be broken down by bacteria in the gut through a process called fermentation.
Fermentation is a metabolic process in which microorganisms, such as bacteria and fungi, break down organic substrates (in this case, carbohydrates) into simpler compounds, often producing gases and other byproducts in the process. In the context of the gut, fermentation primarily occurs in the large intestine, where bacteria ferment undigested carbohydrates that have reached that part of the digestive tract.
During fermentation, bacteria metabolize FODMAPs, producing gases like hydrogen and methane as byproducts. These gases can lead to symptoms such as bloating, flatulence, and abdominal discomfort, particularly in individuals with conditions like irritable bowel syndrome (IBS) or small intestinal bacterial overgrowth (SIBO).
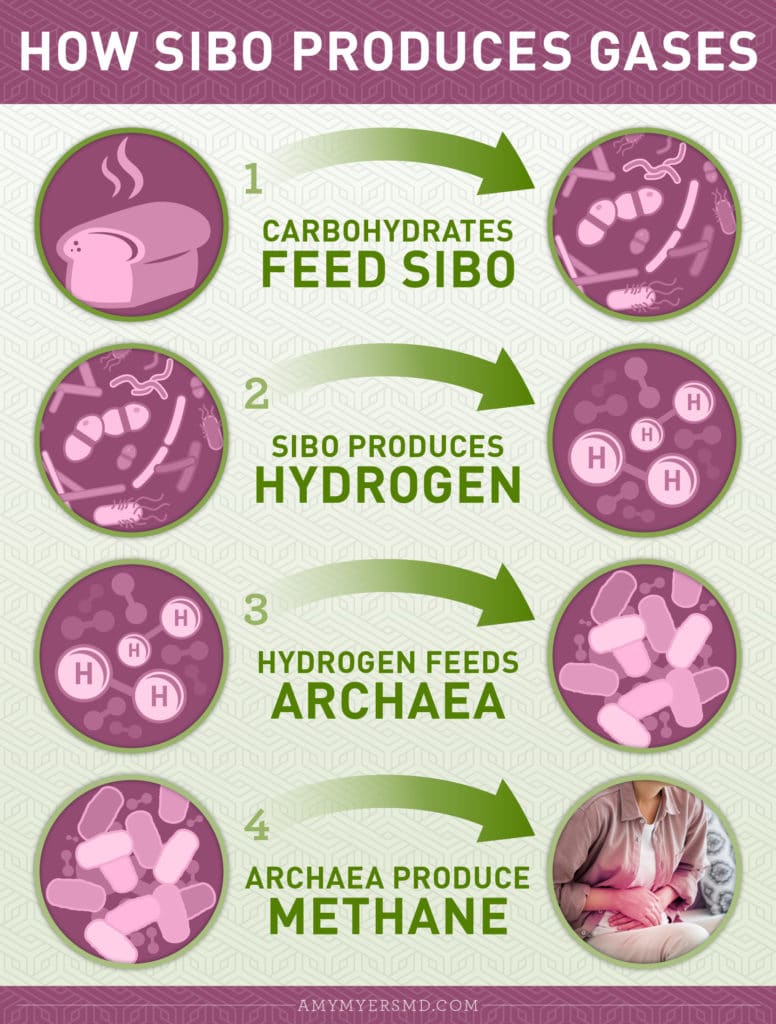
What are gases produced with SIBO?
Hydrogen and methane gases, in particular, play a role in digestive health. In the case of SIBO, excessive production of these gases by bacteria in the small intestine can contribute to symptoms like bloating and abdominal pain. Methane gas, produced by certain types of bacteria, can slow down gut motility, leading to constipation in some individuals.
Reducing FODMAP intake may help alleviate symptoms associated with conditions like IBS and SIBO by reducing the substrate available for fermentation and gas production in the gut. However, the specific dietary approach should be personalized, as individual tolerances to FODMAPs can vary.
Which gut bacteria are associated with SIBO?
Several types of bacteria can be associated with Small Intestinal Bacterial Overgrowth (SIBO).
Some of the common culprits include:
- Escherichia coli (E. coli): While E. coli is normally present in the human gut, overgrowth in the small intestine can lead to SIBO.
- Streptococcus species: Certain species of Streptococcus, such as Streptococcus pneumoniae and Streptococcus pyogenes, can contribute to SIBO when they overgrow in the small intestine.
- Staphylococcus species: Staphylococcus aureus and other Staphylococcus species can also be implicated in SIBO when they proliferate in the small intestine beyond normal levels.
- Enterococcus species: Enterococcus faecalis and Enterococcus faecium are examples of Enterococcus species that may be associated with SIBO.
- Bacteroides species: While Bacteroides are more commonly found in the large intestine, overgrowth in the small intestine can occur and contribute to SIBO.
- Clostridium species: Certain Clostridium species, such as Clostridium difficile, are notorious for causing infections in the gut, but other species can also be involved in SIBO.
- Lactobacillus species: While Lactobacillus species are generally considered beneficial, overgrowth in the small intestine can contribute to SIBO, particularly in individuals with altered gut motility.
These bacteria, when present in excessive amounts in the small intestine, can disrupt the normal digestive processes and lead to symptoms characteristic of SIBO, such as bloating, abdominal pain, diarrhea, and malabsorption of nutrients. Identifying the specific bacteria involved in an individual’s case of SIBO can help guide treatment strategies, which may include dietary modifications, antibiotics, probiotics, and other targeted therapies.
What are the signs and symptoms of SIBO and SIFO?
The signs and symptoms of Small Intestinal Bacterial Overgrowth (SIBO) and Small Intestinal Fungal Overgrowth (SIFO) can overlap but may also have some distinct differences:
Signs and symptoms of SIBO may include:
- Bloating: Excessive gas production by bacteria in the small intestine can lead to bloating, which is often described as feeling uncomfortably full or swollen in the abdomen.
- Abdominal pain or discomfort: Individuals with SIBO may experience abdominal pain or discomfort, which can range from mild to severe and may be crampy or constant.
- Flatulence: Increased gas production can lead to excessive flatulence (passing gas), which may be accompanied by an unpleasant odor.
- Diarrhea or constipation: SIBO can disrupt normal bowel movements, leading to diarrhea, constipation, or a combination of both (alternating diarrhea and constipation).
- Abdominal distension: The abdomen may appear visibly distended or swollen due to gas accumulation.
- Nausea and vomiting: Some individuals with SIBO may experience nausea and, less commonly, vomiting.
- Malabsorption symptoms: SIBO can interfere with the absorption of nutrients, leading to symptoms such as weight loss, fatigue, weakness, and deficiencies in vitamins and minerals.
Signs and symptoms of SIFO may include:
- Similar digestive symptoms: SIFO can cause symptoms similar to those of SIBO, including bloating, abdominal pain, flatulence, diarrhea, constipation, and abdominal distension.
- Oral thrush: SIFO may present with symptoms of oral thrush, such as white patches on the tongue, inner cheeks, or roof of the mouth, along with discomfort or pain.
- Recurrent yeast infections: Individuals with SIFO may experience recurrent yeast infections in the genital area, mouth, or skin folds.
- Fatigue and brain fog: Some people with SIFO may experience fatigue, brain fog, difficulty concentrating, and mood changes.
- Food sensitivities: SIFO can lead to the development of food sensitivities or intolerances, possibly due to inflammation and immune system activation triggered by fungal overgrowth.
It’s important to note that the symptoms of both SIBO and SIFO can vary widely among individuals, and some people may experience only a subset of these symptoms. Additionally, these conditions can coexist, further complicating the clinical picture. Proper diagnosis and management typically involve a combination of clinical evaluation, laboratory tests, and imaging studies, along with targeted treatment approaches tailored to the individual’s specific condition and symptoms.
How to resolve SIBO?
Functional medicine approaches to treating Small Intestinal Bacterial Overgrowth (SIBO) and Small Intestinal Fungal Overgrowth (SIFO) often focus on addressing underlying imbalances in the gut microbiome, supporting digestive function, and alleviating symptoms. Some common treatment strategies for SIBO and SIFO in functional medicine include:
- Dietary modifications: Adjusting the diet is often a cornerstone of treatment for SIBO and SIFO. This may involve eliminating or reducing intake of fermentable carbohydrates (FODMAPs) that feed bacteria and fungi in the small intestine. Additionally, a diet that promotes gut health, such as the Specific Carbohydrate Diet (SCD) or the Low FODMAP Diet, may be recommended.
- Antimicrobial therapy: Antibiotics, herbal antimicrobials, or combination therapies may be used to target and reduce the overgrowth of bacteria or fungi in the small intestine. Antibiotics commonly used for SIBO include rifaximin, neomycin, and metronidazole, while herbal antimicrobials may include berberine, oregano oil, and garlic extract. Antifungal medications or herbs like fluconazole, nystatin, or caprylic acid may be used for SIFO.
- Probiotics: Probiotic supplements containing beneficial bacteria strains, such as Lactobacillus and Bifidobacterium species, may be recommended to help restore balance to the gut microbiome. However, the selection of probiotics should be individualized, as some strains may exacerbate symptoms in certain individuals.
- Prebiotics: Prebiotics are non-digestible fibers that promote the growth and activity of beneficial bacteria in the gut. Prebiotic supplements or dietary sources of prebiotics, such as chicory root, garlic, onions, and Jerusalem artichokes, may be included in the treatment plan.
- Gut motility support: Addressing impaired gut motility, which can contribute to SIBO, may involve using prokinetic agents that stimulate movement through the gastrointestinal tract. Prokinetic medications like low-dose erythromycin, prucalopride, or herbal supplements such as ginger and Iberogast (a combination of herbal extracts) may be prescribed.
- Nutritional support: Nutritional deficiencies resulting from malabsorption in SIBO and SIFO may require supplementation with vitamins, minerals, and other nutrients. This may include vitamin B12, vitamin D, iron, magnesium, and other essential nutrients.
- Stress management and lifestyle modifications: Stress reduction techniques, such as mindfulness meditation, yoga, and relaxation exercises, may help modulate the gut-brain axis and improve gut function. Lifestyle modifications, such as regular exercise, adequate sleep, and avoidance of dietary triggers, can also support overall digestive health.
It’s important to work with a qualified healthcare practitioner, such as a functional medicine doctor or a registered dietitian specializing in gut health, to develop a comprehensive treatment plan tailored to individual needs and preferences. Treatment duration and effectiveness can vary, and close monitoring and adjustments may be necessary to achieve optimal outcomes.
In functional medicine and nutritional therapy, treating SIBO without antibiotics typically involves a comprehensive approach that addresses underlying factors contributing to bacterial overgrowth and promotes gut health. Here’s a solution treatment plan for SIBO without antibiotics:
Dietary Modifications:
-
- Low FODMAP Diet: Adopting a low FODMAP diet can help reduce symptoms associated with SIBO by minimizing fermentable carbohydrates that feed bacterial overgrowth. This involves avoiding high FODMAP foods and focusing on low FODMAP alternatives.
- Specific Carbohydrate Diet (SCD): The SCD restricts complex carbohydrates and focuses on easily digestible foods to starve bacteria in the small intestine. It includes foods like meats, fish, eggs, certain fruits, non-starchy vegetables, and homemade yogurt.
- Elemental Diet: In some cases, an elemental diet may be used as a temporary measure to provide complete nutrition while starving bacteria in the small intestine. This involves consuming only predigested nutrients in the form of a specialized liquid formula for a period of 2-3 weeks.
Prokinetic Agents:
-
- Herbal prokinetics: Certain herbs like ginger, artichoke extract, and motility-enhancing botanicals may be used to improve gut motility and reduce the risk of SIBO recurrence.
- Prescription prokinetics: Prescription medications like low-dose erythromycin or prucalopride may be prescribed by a healthcare provider to stimulate gut motility and prevent bacterial overgrowth.
Nutritional Supplements:
-
- Digestive enzymes: Supplementing with digestive enzymes can aid in the breakdown and absorption of nutrients, supporting digestion and reducing symptoms of bloating and discomfort.
- Gut-healing supplements: Nutrients like glutamine, zinc carnosine, slippery elm, marshmallow root, and aloe vera may help repair and restore the integrity of the gut lining, reducing inflammation and promoting healing.
Probiotics:
-
- Certain strains of probiotics may help rebalance the gut microbiota and reduce bacterial overgrowth in the small intestine.
- Look for probiotic supplements containing strains like Lactobacillus and Bifidobacterium that have been studied for their beneficial effects on gut health.
Lifestyle Modifications:
-
- Stress management: Chronic stress can impair gut function and exacerbate SIBO symptoms. Implement stress-reducing techniques such as mindfulness meditation, yoga, deep breathing exercises, and regular physical activity.
- Adequate sleep: Prioritize quality sleep, aiming for 7-9 hours per night, as insufficient sleep can negatively impact gut health and immune function.
Monitoring and Follow-Up:
-
- Regular monitoring and follow-up with a healthcare provider or a registered dietitian are essential to assess treatment progress, adjust the treatment plan as needed, and address any emerging concerns or challenges.
It’s important to note that while antibiotics are commonly used to treat SIBO, the effectiveness of non-antibiotic approaches may vary depending on individual factors and the severity of the condition. Always consult with a healthcare provider or a qualified practitioner before starting any new treatment regimen, especially if you have underlying health conditions or concerns.
The low FODMAP diet typically involves three phases:
Elimination Phase:
-
- During the elimination phase, the goal is to remove high FODMAP foods from the diet to reduce symptoms associated with SIBO. This phase typically lasts around 2-6 weeks, although the duration may vary depending on individual response and symptom improvement.
- Foods high in fermentable carbohydrates such as fructans (found in wheat, onions, and garlic), oligosaccharides (found in beans, lentils, and some fruits), disaccharides (found in lactose-containing dairy products), monosaccharides (found in certain fruits like apples, pears, and mangoes), and polyols (found in certain fruits, vegetables, and artificial sweeteners) are restricted during this phase.
- Instead, the diet focuses on low FODMAP foods such as certain fruits (e.g., berries, oranges, grapes), vegetables (e.g., spinach, carrots, zucchini), proteins (e.g., meat, fish, eggs), and fats.
- It’s important to ensure adequate nutrient intake during this phase by incorporating a variety of low FODMAP foods and possibly considering supplementation if necessary.
Reintroduction Phase:
-
- In the reintroduction phase, specific high FODMAP foods are systematically reintroduced one at a time to identify individual triggers and tolerance levels.
- Foods are reintroduced gradually, starting with small portions of one FODMAP group at a time, while closely monitoring symptoms. This phase typically lasts several weeks to allow for adequate observation of symptom response.
- Reintroduction may involve testing different types of FODMAPs separately (e.g., fructans, oligosaccharides, lactose, fructose, polyols) to pinpoint which carbohydrates trigger symptoms and in what amounts.
- Keeping a detailed food and symptom diary can be helpful during this phase to track reactions to specific foods and inform future dietary decisions.
Before starting the reintroduction phase of the low FODMAP diet, it’s important to focus on healing the gut and addressing any underlying issues that may contribute to gastrointestinal symptoms.
Here are some steps you might consider:
- Addressing Small Intestinal Bacterial Overgrowth (SIBO): If SIBO is present, it’s crucial to address it before reintroducing high FODMAP foods. This may involve antibiotic therapy, prokinetic agents to improve gut motility, and dietary modifications to reduce bacterial overgrowth.
- Supporting Gut Health with Probiotics: Probiotics are beneficial bacteria that can help restore balance to the gut microbiota and support digestive health. Before reintroducing FODMAPs, you might consider taking a high-quality probiotic supplement containing strains known to promote gut health, such as Lactobacillus and Bifidobacterium species.
- Reducing Gut Inflammation: Certain foods and lifestyle factors can contribute to gut inflammation, exacerbating gastrointestinal symptoms. Focus on consuming anti-inflammatory foods rich in antioxidants, omega-3 fatty acids, and fiber, such as fruits, vegetables, fatty fish, nuts, and seeds. Additionally, manage stress levels, get adequate sleep, and avoid smoking and excessive alcohol intake, as these can all contribute to inflammation.
- Repairing Gut Lining: Supporting gut epithelial integrity is essential for optimal digestive function and overall health. Consider incorporating gut-healing foods and supplements into your diet, such as bone broth, glutamine, slippery elm, marshmallow root, and aloe vera.
- Eliminating Potential Trigger Foods: Before reintroducing FODMAPs, ensure that other potential trigger foods, such as gluten, dairy, and processed foods, are eliminated from your diet. These foods can exacerbate gut inflammation and symptoms in some individuals.
- Optimizing Nutrient Intake: Malabsorption of nutrients due to gut issues like SIBO can lead to deficiencies. Before reintroducing FODMAPs, focus on optimizing your nutrient intake through a balanced diet rich in vitamins, minerals, and macronutrients. Consider consulting with a registered dietitian to ensure you’re meeting your nutritional needs.
By taking these steps to heal and support your gut before reintroducing FODMAPs, you can improve the likelihood of a successful reintroduction phase and better identify your individual trigger foods while minimizing gastrointestinal symptoms. Always consult with a healthcare provider or a registered dietitian before making significant dietary changes, especially if you have underlying health conditions or concerns.
Personalization Phase:
-
- The personalization phase involves tailoring the diet based on individual tolerance levels and identified triggers from the reintroduction phase.
- Once trigger foods are identified, they are either avoided or consumed in small, tolerated amounts while maintaining overall symptom control.
- The goal of this phase is to establish a sustainable and personalized long-term diet plan that minimizes symptoms while allowing for dietary variety and enjoyment.
- It’s important to periodically reassess tolerance levels and make adjustments to the diet as needed, especially in response to changes in symptoms or dietary habits.
Throughout all phases of the low FODMAP diet, it’s recommended to work closely with a healthcare provider or a registered dietitian experienced in managing gastrointestinal disorders to ensure proper guidance, support, and monitoring.
Dr. Amy Myers on SIBO Symptoms:
https://www.amymyersmd.com/article/sibo-small-intestinal-bacterial-overgrowth-symptomsWhat is SIBO?
SIBO, also known as Small Intestinal Bacterial Overgrowth is basically what the name describes. The bacteria in your small intestine get unbalanced and overgrow, instead of living in a balanced state.
In fact, I like to think of your microbiome as a rainforest, with many different species living together in harmony. Together, these species play a vital role in your immune system, thyroid function, bone health, and overall health.
Most of your gut bacteria are meant to be in your large intestine and colon. Here they help break down food, synthesize vitamins, and eliminate waste. However, medications or a poor diet can cause your rainforest to become unbalanced. When this happens, the bacteria normally found in the large intestine and colon overgrow and colonize in your small intestine — leading to SIBO symptoms. What’s more, your gut is naturally lined with mucus that lubricates and protects it. However, an overgrowth of intestinal bacteria can damage your gut’s mucosal lining. Damaged mucus creates an opportunity for bacterial biofilms — or groups of microorganisms that are protected by a layer of protective slime — to attach to your cell wall, making them harder to control.
9 SIBO Symptoms
As I always say: “too much of a good thing can be a bad thing,”. This is true when it comes to small intestinal bacterial overgrowth. Too much good or bad bacterial flora in the small intestine produces a number of gastrointestinal symptoms that interfere with your normal digestive process. SIBO symptoms can range from digestive imbalance to chronic illness and autoimmune conditions. Here are the main symptoms you might experience:
Gas, Bloating, and Diarrhea
Once in the small intestine, the bacteria feed on undigested food and produce either methane or hydrogen, depending on which type of bacteria overgrows. I’ll discuss hydrogen vs methane more in a bit.
Abdominal Pain
Small intestinal bacterial overgrowth causes inflammation in your digestive tract, which can lead to painful symptoms such as abdominal pain and cramping,
Constipation (Much Less Common than Diarrhea)
SIBO can disrupt the natural gut flora, which affects your ability to eliminate waste and lead to constipation.
Irritable Bowel Syndrome (IBS) or Inflammatory Bowel Disease (IBD)
SIBO symptoms are extremely similar to those of IBS. In fact, one study proved that nearly 80% of people with IBS also had SIBO. When the SIBO was treated, nearly half of the patients experienced an improvement in their IBS.
Food Intolerances
Intolerances such as gluten, casein, lactose, fructose, and particularly histamine intolerance: SIBO causes dysmotility, which inhibits your ability to properly digest foods and allows both food and bacteria to sit in your digestive system for longer, further exacerbating inflammation.
Leaky gut: inflammation in your gut leads to intestinal permeability, where the tight junctions holding your intestinal wall together become loose. When you have leaky gut, toxins, microbes, and undigested food particles can escape through the holes and into your bloodstream, where your immune system marks them as pathogens and attacks them.
Chronic Illnesses
Illnesses such as fibromyalgia, chronic fatigue syndrome, diabetes, neuromuscular disorders, and autoimmune diseases: as your gut remains leaky and more and more particles escape into your bloodstream, your immune system sends out wave after wave of inflammation.
Eventually, it becomes over-stressed and begins firing less accurately. What’s more, many particles that are now flooding your bloodstream look like your body’s own tissues.
Your immune system creates antibodies against these substances, which mistakenly attack your tissues in a phenomenon called molecular mimicry.
Vitamin and Mineral Deficiencies
Deficiencies, including vitamins A, B12, D, and E: when your gut lining is impaired, your ability to absorb nutrients is impacted. So even if you’re getting plenty of vitamins and minerals in your diet, they might be passing straight through your body without providing any benefits and creating nutritional deficiencies.
Fat Malabsorption
When you have SIBO, the bile acids responsible for the breakdown and absorption of fat are deficient, resulting in a pale-colored stool that is also bulky and malodorous.
Rosacea and Other Skin Rashes
Rosacea and other skin rashes: Small intestinal bacterial overgrowth damages the gut lining, which leads to the release of cytokines (regulators of host immune responses that promote inflammatory reactions) resulting in skin inflammation.
What Causes SIBO?
After enzymes break down our food, it travels through our digestive system from the stomach to the small intestine.
In a healthy gut, bacteria gets passed through the digestive tract along with our food to the colon.
Unfortunately, this process can be disrupted by a number of risk factors, including:1
- Damaged nerves or muscles in the gut resulting in leftover bacteria in the small intestine.
- For example, diabetes mellitus and scleroderma can both affect the muscles in the gut, leaving room for SIBO to develop.
- Physical obstructions in the gut, such as scarring from surgeries or Crohn’s disease and diverticula (tiny pouches that can form in the wall of the small intestine) can collect bacteria instead of passing it on to the colon, where it belongs.
- Medications that influence or disrupt the normal gut flora including antibiotics, acid-blocking drugs, and steroids.
- A diet high in sugar, refined carbohydrates, alcohol, and other high-carb foods you eat or drink.
How SIBO Produces Hydrogen & Methane Gas
While colonizing in your small intestine, the group of overgrown bacteria can thrive by feeding off the undigested food passing through. This process of fermenting carbohydrates produces hydrogen. Hydrogen can feed the single-celled organisms in your small intestine called archaea, which then produces methane. All that excess gas in your gastrointestinal tract is what contributes to the severe bloating people experience while dealing with SIBO, in addition to a whole host of digestive, mood, and chronic issues.
Do You Have SIBO Symptoms, or IBS?
Because of the many ways in which SIBO symptoms manifest in different people — sometimes showing no physical signs whatsoever — these symptoms often go undiagnosed. An estimated 6-15% of healthy, asymptomatic people, and roughly 80% of people with IBS, actually suffer from small intestinal bacterial overgrowth.2
SIBO Testing
Before I explain the most effective and accurate lab tests for SIBO3, let’s recap the two different types of small intestinal bacterial overgrowth so that you can understand their role in testing.
Hydrogen vs Methane
As I explained earlier, when you have an overgrowth of bacteria in your small intestine, the carbs you eat can ferment before they are broken down. This fermentation process releases hydrogen gas, so people who experience SIBO symptoms often exhibit elevated levels of hydrogen in their GI tract.
Hydrogen SIBO
Hydrogen dominant or hydrogen SIBO is diagnosed by a sufficient rise in hydrogen on a breath test. This form of bacterial overgrowth is also referred to as diarrhea-prone SIBO, as the by-products of carbohydrate fermentation create an osmosis-like effect, drawing water into the bowel and causing diarrhea.
What’s more, hydrogen SIBO can cause damage to your gut’s mucosal lining, creating a lactase deficiency. Lactase is the enzyme we use to break down and digest lactose. This is another reason why sudden food intolerances are a sign of an underlying gut infection.
Methane SIBO
SIBO can also cause an increase in methane levels. As the hydrogen feeds single-cell organisms in your gut called archaea, they produce methane. This can reduce your hydrogen levels which explains why you can have a false negative hydrogen breath test result and still have methane SIBO.
If you have small intestinal bacterial overgrowth and are dealing with constipation as your main symptom, you likely have methane SIBO.
You ideally want your lab testing to identify which type (hydrogen or methane SIBO) you have as the two respond differently to different treatment options.
SIBO Lab Testing Options
1. Breath Test
This is certainly the gold standard when it comes to a SIBO test. It is the most accurate and determines if the bacterial overgrowth is hydrogen or methane dominant. However, it can be a bit cumbersome.
For this test, you need to fast for 12 hours and breathe into a small balloon to measure baseline levels of hydrogen and methane. Then, you ingest a precise amount of sugar to feed the bacteria and repeat breath samples every 15 minutes for 3 or more hours to see if levels of hydrogen or methane increase.
If your hydrogen levels are high then you likely have hydrogen SIBO. However, just because one gas is dominant doesn’t mean that only one type of gas is present. You can have both types of gas present, one is just more prevalent.
I recommend the Lactulose Breath Test from Aerodiagnostics.
2. Organix Dysbiosis Test
This functional medicine SIBO test runs urine for by-products of yeast or bacteria in the small intestine. If your small intestine is housing a yeast or bacterial overgrowth, byproducts will appear in your urine, indicating their presence. This test is much easier for patients and only requires a single urine specimen. Yet, it does not determine whether your bacterial overgrowth is hydrogen or methane-dominant.
3. Comprehensive Stool Test
This is also a functional medicine test looking at the flora of the large intestines. If I see elevated levels of all good bacteria, I suspect SIBO. I often use stool testing to test for multiple gut infections at one time. This is because there were usually multiple, overlapping gut issues such as Candida overgrowth, small intestinal bacterial overgrowth, and parasites.
4. SIBO Symptoms Checklist
Using a patient’s health history, lifestyle factors, and the list of common symptoms above, I am often able to make a diagnosis by listening to the patient’s symptoms.
3-Step Protocol for Treating SIBO
Treating your bacterial overgrowth is a 3-step approach that works to eliminate the overgrowth and restore your gut’s natural balance. My SIBO Breakthrough™ Program is a step-by-step process to help you beat small intestinal bacterial overgrowth for good. In it, you find all the information you need to get control over the overgrowth. With the SIBO Breakthrough™ Program, not only do you get information, supplements, and a solution, you also get the support you need to take on these three steps. Check out my video below:
Step 1: Starve the Overgrown Bacteria
Starve the overgrown bacteria by removing the foods that feed it from your diet.
This means cutting all sugar and alcohol and limiting carbohydrates such as fruit, starchy vegetables, grains, and legumes.
While some inflammatory foods can be reintroduced after getting your gut back in balance, I recommend a SIBO diet that ditches gluten and dairy for good, particularly if you have an autoimmune or thyroid condition.
Step 2: Attack the Bacteria
In my clinic, I typically used the antibiotics Xifaxan and Neomycin to attack the bad bacteria. Xifaxan is more effective with hydrogen-dominant SIBO and Neomycin with methane SIBO. These antibiotics kill the pathogenic bacteria with the least amount of disruption to the good bacteria in your microbiome.
If starving the overgrowth and attacking the bacteria have little effect on your SIBO symptoms, it could be because a biofilm has formed around the overgrown bacteria, making it more difficult to eliminate. In these cases, I recommend treating bacterial overgrowth with a biofilm disruptor such as Microb-Clear®. It is a blend of magnesium caprylate, berberine, and extracts from tribulus, sweet wormwood, barberry, bearberry, and black walnut. These ingredients work to kill off the bacteria naturally.
The ingredients are not as harsh as broad-spectrum prescription antibiotics which can wipe out good and bad bacteria alike. Microb-Clear® is a natural and gentle way to support your journey to optimal health.
Step 3: Restore Your Good Bacteria
The final step is to restore the good bacteria in your gut. This will help support a strong immune system, optimal digestion, and nutrient absorption. Moreover, when it comes to small intestinal bacterial overgrowth you want to be particularly careful. Certain probiotics can add fuel to the fire and exacerbate your SIBO symptoms.
The Problem with Most Probiotics
When you have an overgrowth of bacteria in your small intestine, it is often lactobacillus or bifidobacterium species. The majority of probiotic supplements contain these species, so using them adds to the bacteria in your small intestine.
Consequently, one clue that you may have small intestinal bacterial overgrowth is that probiotics containing lactobacillus or bifidobacterium exacerbate your symptoms.
Why Soil-Based Probiotics Are Best for SIBO
Soil-based probiotics don’t colonize the small intestine or feed the bacteria already growing there. In short, they do not contain lactobacillus or bifidobacterium strains, yet provide all the benefits of a probiotic.
These steps, supplements, and more can all be found in my SIBO Breakthrough™ Program.
Using this tried and true method, you can combat your symptoms of SIBO and take back your health in the long term!
SIBO Symptoms FAQWhat is the best diet to treat Small Intestinal Bacterial Overgrowth?
A SIBO diet minimizes fruit intake and includes plenty of non-starchy vegetables, leafy greens, lean proteins, and healthy fats.
When should I get tested for SIBO?
If you have been treated for certain diseases (such as IBS, diabetes, chronic fatigue, fibromyalgia, or another autoimmune disease) and you haven’t experienced much or any relief, I suggest you get tested. If you do have it, treating it is likely to lead to vast improvements in your symptoms.
Can SIBO Symptoms away on their own?
Small intestinal bacterial overgrowth needs to be addressed for it to go away.
Removing toxic and inflammatory foods from your diet and taking gut-supporting nutrients will help mitigate your symptoms.
Article Sources
- What is Small Intestinal Bacterial Overgrowth (SIBO). Health Insight.
- Small Intestinal Bacterial Overgrowth: A Comprehensive Review. Andrew C. Dukowicz, MD, Brian E. Lacy, PhD, MD, and Gary M. Levine, MD. NCBI. 2007.
- Top Gut Secrets: How to Test for Dysbiosis, SIBO, and Leaky Gut. Sara Gottfried, MD. Dr. Sara Gottfried, MD. 2015.