Are you struggling to get your vibrant self back again!?
Test and not guess if you have HPA Axis DYS-Function and IM-Balance… do you have high or low cortisol – and ask WHY?
As I prepare for a few podcast interview on my personal story “LIFE IS NOT A RACE… IT IS A JOURNEY” and an online summit on chronic stress, I had to go back in time as my journey with overcoming breakdown and burnout from chronic stress started in 2013!
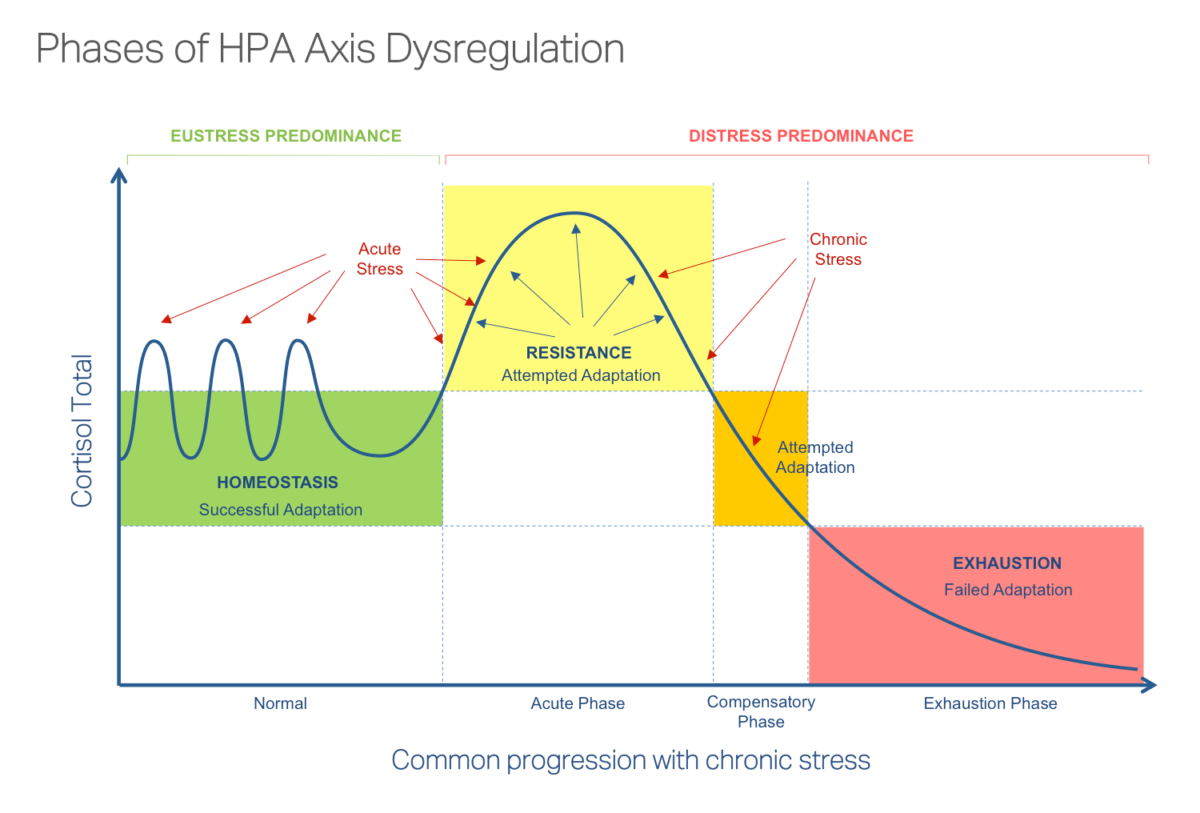
Progression of HPA Axis Dysfunction: From High Cortisol to Low Cortisol Phases
The HPA axis (hypothalamic-pituitary-adrenal axis) plays a critical role in regulating the body’s response to stress. When the body experiences stress, whether external (e.g., emotional stress, environmental stress) or internal (e.g., chronic inflammation, nutrient deficiencies), the HPA axis is activated, leading to the release of cortisol. Prolonged or chronic stress can disrupt the normal functioning of the HPA axis, leading to a progression of dysfunction that can ultimately result in low cortisol levels. This progression typically unfolds in phases, from initially high cortisol levels to eventual cortisol depletion.
Phase 1: Initial Stress Response – High Cortisol
In response to acute or chronic stress, the HPA axis is activated. Stressors (whether external like work pressure or internal like inflammation or blood sugar imbalances) trigger the hypothalamus to release corticotropin-releasing hormone (CRH). This, in turn, stimulates the pituitary gland to release adrenocorticotropic hormone (ACTH), which signals the adrenal glands to produce and release cortisol.
Cortisol serves several functions in the body, including:
- Increasing blood sugar for quick energy.
- Suppressing non-essential functions (like digestion and immune response) to prioritize dealing with the immediate stressor.
- Enhancing brain function to improve focus and alertness.
In the short term, this is a protective mechanism to help the body deal with stress. However, if stress continues over a long period, cortisol remains elevated, leading to negative consequences.
Symptoms of High Cortisol:
- Increased energy and alertness (temporary boost)
- Increased blood sugar (leading to weight gain, especially abdominal fat)
- Poor sleep quality (due to elevated cortisol at night)
- Reduced digestion (due to blood flow being redirected away from the digestive system)
- Weakened immune system (chronic inflammation suppression)
- Irritability, anxiety, or agitation
Phase 2: Prolonged Stress – Dysregulation of the HPA Axis
With chronic exposure to stress, the HPA axis begins to become dysregulated. The body is in a continuous state of fight-or-flight, leading to persistently elevated cortisol levels. The adrenal glands may become overstimulated, but eventually, they can start to fatigue from the constant demand for cortisol production.
In this phase, the body starts to experience a stress overload, and the initial response of high cortisol no longer serves as an effective defense. The body’s feedback loop (which regulates cortisol levels through a negative feedback mechanism) becomes impaired. This dysregulation results in excessive cortisol secretion, leading to the following:
- Increased fat storage, particularly abdominal fat, due to cortisol’s role in stimulating insulin and promoting fat storage.
- Impaired metabolic function, including insulin resistance and blood sugar dysregulation.
- Gut dysfunction (leading to leaky gut), as cortisol impairs digestion and blood flow to the gut.
- Depleted immune function and chronic inflammation, increasing susceptibility to infections and autoimmune conditions.
Symptoms of Prolonged High Cortisol:
- Persistent fatigue despite feeling wired or on edge
- Digestive issues like bloating, constipation, or diarrhea
- Increased belly fat and difficulty losing weight
- Sleep disturbances (difficulty falling or staying asleep)
- Elevated heart rate and high blood pressure
- Mood swings, anxiety, or depression
Phase 3: Burnout and Adrenal Fatigue – Low Cortisol
After prolonged exposure to stress, the adrenal glands can become fatigued, and the body enters a state where cortisol levels begin to decline. This phase is often referred to as adrenal fatigue or HPA axis dysfunction.
In this phase, the adrenal glands no longer produce cortisol in sufficient quantities because they’ve become overwhelmed by the constant demand. This leads to low cortisol levels and an inability to mount an adequate stress response.
At this stage, the body struggles to recover and maintain normal functions, as it lacks the energy and regulatory mechanisms to restore balance.
Symptoms of Low Cortisol:
- Chronic fatigue or extreme tiredness, even after rest
- Low motivation or lack of energy to handle normal activities
- Brain fog or difficulty concentrating
- Poor stress resilience, feeling overwhelmed easily
- Low blood pressure or dizziness when standing up
- Frequent infections due to suppressed immune function
- Hormonal imbalances, including low thyroid function, menstrual irregularities, or low libido
Connection to Metabolic Chaos
The progression from high cortisol to low cortisol is a key feature of Metabolic Chaos. This refers to the systemic dysfunction that results when the body’s hormonal, metabolic, immune, and digestive systems become imbalanced due to prolonged stress and cortisol dysregulation.
-
Metabolic Disruption:
- Chronic high cortisol leads to insulin resistance, fat storage, and blood sugar imbalances, contributing to weight gain (especially around the abdomen) and difficulty losing weight.
- Low cortisol impairs the stress response, reducing the body’s ability to maintain balance and respond to stressors effectively, which can lead to burnout and fatigue.
-
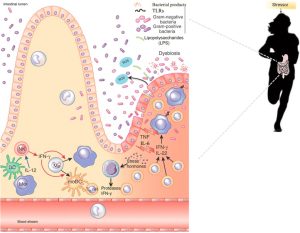
Gut Dysfunction:
- High cortisol impairs digestive function by reducing blood flow to the gut and disrupting gut permeability. This can lead to leaky gut, where the intestinal lining becomes more porous, allowing toxins and undigested food particles to leak into the bloodstream, causing inflammation and immune system activation.
- Over time, this dysfunction can contribute to autoimmune diseases and systemic inflammation.
-
Immune System Dysfunction:
- Prolonged high cortisol suppresses the immune system, leaving the body vulnerable to chronic infections and autoimmune conditions.
- As cortisol drops during adrenal fatigue, the immune system remains suppressed, further increasing the risk of illness and inflammation.
-
Hormonal Imbalances:
- High cortisol can disrupt the balance of other hormones, including thyroid hormones (leading to hypothyroidism), sex hormones (leading to PMS, low libido, or menstrual irregularities), and insulin (leading to insulin resistance).
The WHOLE You: How Chronic Stress Impacts Every System
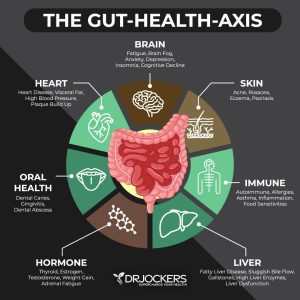
The HPA axis dysfunction impacts the WHOLE you, from the inside out, by disrupting the endocrine, digestive, immune, and nervous systems:
- Hormonal Imbalance: Chronic stress and cortisol dysregulation lead to problems with adrenal, thyroid, sex hormones, and insulin. This affects everything from metabolism to mood and reproductive health.
- Metabolic Dysfunction: Insulin resistance, fat storage, and difficulties with weight management are direct results of dysregulated cortisol levels.
- Digestive Dysfunction: Chronic stress causes leaky gut, impaired digestion, and nutrient deficiencies, all of which contribute to gut dysbiosis and immune dysfunction.
- Immune Dysfunction: Cortisol’s role in suppressing inflammation becomes a problem when it persists for too long, contributing to chronic inflammation, autoimmune disease, and poor immune defense.
- Mental and Emotional Health: The dysregulation of cortisol affects neurotransmitter production (e.g., serotonin, dopamine), leading to mood disturbances, anxiety, and depression.
Investigating Metabolic Chaos as FDN Practitioners
As FDN Practitioners, we help uncover the hidden stressors that contribute to HPA axis dysfunction and Metabolic Chaos. Through comprehensive testing and functional health assessments, we can identify factors such as:
- Chronic internal stress (e.g., inflammation, gut issues, nutrient deficiencies)
- External stressors (e.g., work, relationships, environmental toxins)
- Hormonal imbalances, blood sugar dysregulation, and digestive dysfunction
By addressing these root causes through personalized nutrition, lifestyle changes, and targeted supplementation, we guide clients through the process of rebalancing the HPA axis, restoring cortisol levels, and rebuilding their health from the inside out. This allows the body to regain its resilience and return to a state of homeostasis, where metabolic systems function optimally, energy is restored, and the body can recover from stress effectively.
Debbie Potts’ struggle with overcoming burnout and breakdown from HPA Axis Dysfunction, despite sharing her personal story and writing the books Life is Not a Race, It is a Journey and The WHOLESTIC Method Manual, can be understood as the intersection of her relentless pursuit of performance, her identity as a high-achieving individual, and the complex nature of chronic stress.
1. High-Performance Culture and Personal Identity
Debbie, as a driven and high-performing individual, has always been committed to pushing herself to the limits, particularly in her triathlon and endurance athlete pursuits. Her identity was deeply intertwined with achieving exceptional results, which often meant sacrificing recovery, rest, and listening to her body. This drive for performance and “doing” can sometimes create a barrier to the necessary internal signals of stress and exhaustion. As someone who spent years training for top-tier events, it’s understandable that the external success masked the internal breakdown until it became overwhelming.
2. Chronic Stress and Cumulative Impact
HPA axis dysfunction develops gradually, particularly in high-stress environments, and it often takes years of chronic stress exposure to fully manifest. Even though Debbie shared her story and journey publicly, the cumulative effect of years of pushing her body beyond its capacity, combined with the physical and emotional toll, contributed to her eventual burnout. HPA axis dysfunction is insidious — it often starts with high cortisol levels in response to stress and can later result in a decrease in cortisol production (adrenal fatigue). Even if one is aware of the symptoms or has researched stress management techniques, the body’s adaptation to chronic stress is often not immediate, and recovery is a long, multifactorial process.
3. The Disconnect Between Knowledge and Implementation
Debbie’s journey includes knowing the solutions — through her training, books, and certifications — but even knowing the right steps to take doesn’t necessarily make implementing them easy. This is particularly true when a person is ingrained in a high-performance lifestyle. The act of doing more becomes ingrained, and sometimes, despite knowing the importance of rest, relaxation, and recovery, it can be difficult to prioritize those things over performance goals. In addition, “Metabolic Chaos” from chronic stress impacts different systems, including the adrenal glands, thyroid, immune system, and gut, all of which require time and deep focus to heal. Overcoming burnout often involves dismantling long-held beliefs around personal identity, which can be hard even with the best knowledge and intention.

4. HPA Axis Dysfunction’s Complexity
HPA Axis dysfunction itself is complex, often presenting with symptoms like fatigue, brain fog, low energy, and mood swings — issues that can overlap with other conditions. Even after recognizing HPA Axis dysfunction and burnout, the process of healing requires slow and steady adjustments, both physiologically and emotionally. It’s not a one-time fix but a gradual recovery process that can take months or years to stabilize the adrenal system and return cortisol rhythms to normal.
5. The Paradox of Healing
Sometimes, when one has spent a lifetime in a high-stress environment, healing can feel counterintuitive. Debbie may have found herself facing a paradox: to truly heal, she had to embrace rest and accept the pace of recovery, which could feel uncomfortable after years of pushing through. It’s a shift from doing to being — something that goes against the grain of a high-achieving mindset. Additionally, the emotional and psychological aspects of this process may not have been fully addressed at first, even though her book and methodology guide others. This is common because healing from HPA axis dysfunction also requires personal introspection, emotional processing, and acceptance of vulnerability, which can take time to integrate fully into one’s lifestyle.
6. Healing Is a Nonlinear Process
The healing journey from burnout and HPA axis dysfunction is non-linear. There will be setbacks, and improvement often comes in waves. There may have been moments where, despite the tools Debbie shared with others, she still struggled with implementing them in her own life, facing times of stress that overwhelmed her ability to recover. Even though Debbie wrote The WHOLESTIC Method Manual, which offers structured solutions to metabolic chaos, the reality is that deep healing is more than just following a protocol — it’s about integrating all aspects of life (nutrition, movement, sleep, emotional health, and mindset) and changing deeply ingrained patterns, which takes time.
In summary, Debbie Potts’ struggle with overcoming burnout and HPA Axis Dysfunction comes down to a combination of:
- The high-performance mentality and deeply ingrained habits.
- The long-term cumulative impact of chronic stress.
- The challenge of translating knowledge into consistent practice, particularly when one has always been used to “doing more.”
- The nonlinear nature of healing, where setbacks and emotional processing are part of the recovery.
Despite her knowledge, personal experience, and expertise, overcoming burnout required deep personal work, acceptance, and a commitment to a pace of recovery that may have felt counterintuitive to her previous high-achieving self.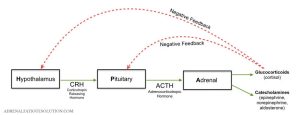
Progression of HPA Axis Dysfunction: From High Cortisol to Low Cortisol Phases
The HPA axis (hypothalamic-pituitary-adrenal axis) plays a critical role in regulating the body’s response to stress. When the body experiences stress, whether external (e.g., emotional stress, environmental stress) or internal (e.g., chronic inflammation, nutrient deficiencies), the HPA axis is activated, leading to the release of cortisol. Prolonged or chronic stress can disrupt the normal functioning of the HPA axis, leading to a progression of dysfunction that can ultimately result in low cortisol levels. This progression typically unfolds in phases, from initially high cortisol levels to eventual cortisol depletion.
Phase 1: Initial Stress Response – High Cortisol
In response to acute or chronic stress, the HPA axis is activated. Stressors (whether external like work pressure or internal like inflammation or blood sugar imbalances) trigger the hypothalamus to release corticotropin-releasing hormone (CRH). This, in turn, stimulates the pituitary gland to release adrenocorticotropic hormone (ACTH), which signals the adrenal glands to produce and release cortisol.
Cortisol serves several functions in the body, including:
- Increasing blood sugar for quick energy.
- Suppressing non-essential functions (like digestion and immune response) to prioritize dealing with the immediate stressor.
- Enhancing brain function to improve focus and alertness.
In the short term, this is a protective mechanism to help the body deal with stress. However, if stress continues over a long period, cortisol remains elevated, leading to negative consequences.
Symptoms of High Cortisol:
- Increased energy and alertness (temporary boost)
- Increased blood sugar (leading to weight gain, especially abdominal fat)
- Poor sleep quality (due to elevated cortisol at night)
- Reduced digestion (due to blood flow being redirected away from the digestive system)
- Weakened immune system (chronic inflammation suppression)
- Irritability, anxiety, or agitation
Phase 2: Prolonged Stress – Dysregulation of the HPA Axis
With chronic exposure to stress, the HPA axis begins to become dysregulated. The body is in a continuous state of fight-or-flight, leading to persistently elevated cortisol levels. The adrenal glands may become overstimulated, but eventually, they can start to fatigue from the constant demand for cortisol production.
In this phase, the body starts to experience a stress overload, and the initial response of high cortisol no longer serves as an effective defense. The body’s feedback loop (which regulates cortisol levels through a negative feedback mechanism) becomes impaired. This dysregulation results in excessive cortisol secretion, leading to the following:
- Increased fat storage, particularly abdominal fat, due to cortisol’s role in stimulating insulin and promoting fat storage.
- Impaired metabolic function, including insulin resistance and blood sugar dysregulation.
- Gut dysfunction (leading to leaky gut), as cortisol impairs digestion and blood flow to the gut.
- Depleted immune function and chronic inflammation, increasing susceptibility to infections and autoimmune conditions.
Symptoms of Prolonged High Cortisol:
- Persistent fatigue despite feeling wired or on edge
- Digestive issues like bloating, constipation, or diarrhea
- Increased belly fat and difficulty losing weight
- Sleep disturbances (difficulty falling or staying asleep)
- Elevated heart rate and high blood pressure
- Mood swings, anxiety, or depression
Phase 3: Burnout and Adrenal Fatigue – Low Cortisol
After prolonged exposure to stress, the adrenal glands can become fatigued, and the body enters a state where cortisol levels begin to decline. This phase is often referred to as adrenal fatigue or HPA axis dysfunction.
In this phase, the adrenal glands no longer produce cortisol in sufficient quantities because they’ve become overwhelmed by the constant demand. This leads to low cortisol levels and an inability to mount an adequate stress response.
At this stage, the body struggles to recover and maintain normal functions, as it lacks the energy and regulatory mechanisms to restore balance.
Symptoms of Low Cortisol:
- Chronic fatigue or extreme tiredness, even after rest
- Low motivation or lack of energy to handle normal activities
- Brain fog or difficulty concentrating
- Poor stress resilience, feeling overwhelmed easily
- Low blood pressure or dizziness when standing up
- Frequent infections due to suppressed immune function
- Hormonal imbalances, including low thyroid function, menstrual irregularities, or low libido
Here’s a comparison chart of the signs and symptoms of high cortisol vs. low cortisol:
| Signs/Symptoms | High Cortisol | Low Cortisol |
|---|---|---|
| Energy Levels | High energy, anxiety, or jitteriness in the short term, but crashes later | Chronic fatigue, feeling sluggish or drained, difficulty getting out of bed |
| Sleep Patterns | Difficulty falling asleep, disturbed sleep, insomnia | Sleep disturbances, waking up often during the night, early morning waking |
| Mood | Irritability, anxiety, feeling wired, mood swings, stress-induced mood swings | Depression, irritability, brain fog, apathy, feeling emotionally numb |
| Appetite | Increased cravings, especially for salty, sugary, or fatty foods | Low appetite, trouble maintaining normal eating habits |
| Weight | Weight gain, especially around the abdomen, “stress belly” | Weight loss, muscle wasting, or difficulty maintaining weight |
| Immune System | Increased susceptibility to infections, slower recovery from illness | Weakened immune system, prone to illness, slow recovery from sickness |
| Cognitive Function | Mental clarity or focus, but can become impaired with prolonged stress | Difficulty concentrating, brain fog, memory problems |
| Muscle and Joints | Muscle tension, jaw clenching, headaches, tightness in the body | Muscle weakness, joint pain, feeling of physical weakness |
| Blood Pressure | Elevated blood pressure, hypertension | Low blood pressure, dizziness, lightheadedness when standing up |
| Libido | Decreased libido due to prolonged stress | Decreased libido due to exhaustion or hormonal imbalances |
| Skin | Thinning skin, bruising easily, acne, stretch marks | Dry skin, pale complexion, thinning or brittle hair |
| Salt and Fluid Balance | Increased salt cravings, water retention, bloating | Low sodium levels, dehydration, salt cravings in severe cases |
| Hormonal Imbalance | Irregular periods in women, reduced fertility, hormone imbalance | Irregular periods, infertility, loss of menstrual cycle (amenorrhea) |
| Heart Health | Increased heart rate, palpitations, tachycardia | Fatigue, fainting, feeling of heart palpitations or arrhythmia |
| Gastrointestinal Issues | Digestive issues (gas, bloating, acid reflux), upset stomach | Nausea, lack of appetite, bloating, low digestive function |
Key Differences:
- High cortisol tends to manifest in physical signs of stress, such as muscle tension, weight gain (especially in the abdomen), and digestive issues like bloating and acid reflux.
- Low cortisol often leads to a sense of exhaustion, low energy, weight loss, and difficulty recovering from illness, as the body’s systems struggle to handle stress.
This comparison helps highlight the body’s complex response to chronic stress, with the HPA axis dysfunction affecting multiple systems in the body in different ways depending on whether cortisol levels are elevated or depleted.

Connection to Metabolic Chaos
The progression from high cortisol to low cortisol is a key feature of Metabolic Chaos. This refers to the systemic dysfunction that results when the body’s hormonal, metabolic, immune, and digestive systems become imbalanced due to prolonged stress and cortisol dysregulation.
-
Metabolic Disruption:
- Chronic high cortisol leads to insulin resistance, fat storage, and blood sugar imbalances, contributing to weight gain (especially around the abdomen) and difficulty losing weight.
- Low cortisol impairs the stress response, reducing the body’s ability to maintain balance and respond to stressors effectively, which can lead to burnout and fatigue.
-
Gut Dysfunction:
- High cortisol impairs digestive function by reducing blood flow to the gut and disrupting gut permeability. This can lead to leaky gut, where the intestinal lining becomes more porous, allowing toxins and undigested food particles to leak into the bloodstream, causing inflammation and immune system activation.
- Over time, this dysfunction can contribute to autoimmune diseases and systemic inflammation.
-
 Immune System Dysfunction:
Immune System Dysfunction:- Prolonged high cortisol suppresses the immune system, leaving the body vulnerable to chronic infections and autoimmune conditions.
- As cortisol drops during adrenal fatigue, the immune system remains suppressed, further increasing the risk of illness and inflammation.
-
Hormonal Imbalances:
- High cortisol can disrupt the balance of other hormones, including thyroid hormones (leading to hypothyroidism), sex hormones (leading to PMS, low libido, or menstrual irregularities), and insulin (leading to insulin resistance).
The WHOLE You: How Chronic Stress Impacts Every System
The HPA axis dysfunction impacts the WHOLE you, from the inside out, by disrupting the endocrine, digestive, immune, and nervous systems:
- Hormonal Imbalance: Chronic stress and cortisol dysregulation lead to problems with adrenal, thyroid, sex hormones, and insulin. This affects everything from metabolism to mood and reproductive health.
- Metabolic Dysfunction: Insulin resistance, fat storage, and difficulties with weight management are direct results of dysregulated cortisol levels.
- Digestive Dysfunction: Chronic stress causes leaky gut, impaired digestion, and nutrient deficiencies, all of which contribute to gut dysbiosis and immune dysfunction.
- Immune Dysfunction: Cortisol’s role in suppressing inflammation becomes a problem when it persists for too long, contributing to chronic inflammation, autoimmune disease, and poor immune defense.
- Mental and Emotional Health: The dysregulation of cortisol affects neurotransmitter production (e.g., serotonin, dopamine), leading to mood disturbances, anxiety, and depression.
Investigating Metabolic Chaos as FDN Practitioners
As FDN Practitioners, we help uncover the hidden stressors that contribute to HPA axis dysfunction and Metabolic Chaos. Through comprehensive testing and functional health assessments, we can identify factors such as:
- Chronic internal stress (e.g., inflammation, gut issues, nutrient deficiencies)
- External stressors (e.g., work, relationships, environmental toxins)
- Hormonal imbalances, blood sugar dysregulation, and digestive dysfunction
By addressing these root causes through personalized nutrition, lifestyle changes, and targeted supplementation, we guide clients through the process of rebalancing the HPA axis, restoring cortisol levels, and rebuilding their health from the inside out. This allows the body to regain its resilience and return to a state of homeostasis, where metabolic systems function optimally, energy is restored, and the body can recover from stress effectively.
Signs and Symptoms of Low Cortisol:
Low cortisol is often linked with adrenal insufficiency or Addison’s disease. Symptoms include:
- Fatigue: Persistent tiredness, especially in the morning.
- Low blood pressure: Feeling lightheaded or dizzy, especially when standing up.
- Weakness: Particularly in the muscles and joints.
- Salt cravings: Due to low aldosterone levels.
- Hypoglycemia: Low blood sugar, causing shakiness, irritability, or dizziness.
- Decreased libido: Low sex drive.
- Depression or mood swings: Emotional lows and irritability.
- Unexplained weight loss: Despite normal or increased appetite.
- Poor recovery: Difficulty recovering from illness or physical activity.
Signs and Symptoms of High Cortisol:
High cortisol is often a result of chronic stress or sometimes it could be Cushing’s syndrome.
High Cortisol Symptoms include:
- Increased abdominal fat: Particularly around the waist and upper back.
- Thinning skin: Fragile skin that bruises easily.
- Muscle weakness: Especially in the arms and legs.
- Sleep disturbances: Trouble falling asleep or staying asleep.
- Increased anxiety or irritability: Feeling on edge or easily upset.
- Weight gain: Especially in the face (moon face) and upper back (buffalo hump).
- High blood pressure: Elevated blood pressure due to fluid retention and vascular effects.
- Poor immune function: Increased susceptibility to infections and illnesses.
- Memory and concentration issues: Brain fog or difficulties with focus and recall.
- Digestive issues: Such as bloating, indigestion, or constipation.
HPA Axis Progression:
The Hypothalamic-Pituitary-Adrenal (HPA) axis is the system that controls your body’s response to stress. Here’s a breakdown of its progression:
-
Acute Stress Response (Fight or Flight):
In response to a perceived stressor, the hypothalamus releases corticotropin-releasing hormone (CRH), prompting the pituitary gland to release adrenocorticotropic hormone (ACTH). This triggers the adrenal glands to release cortisol. This helps the body manage short-term stress by increasing alertness and glucose availability. -
Chronic Stress:
With ongoing stress, the HPA axis becomes overstimulated, leading to prolonged cortisol release. The body attempts to keep up with the stress demand, but eventually, cortisol levels may become dysregulated, either too high or too low. -
Adrenal Fatigue (though debated in modern medicine):
When the adrenal glands become worn out from prolonged high cortisol secretion, they may struggle to produce adequate cortisol. This leads to symptoms of low cortisol, such as fatigue and low energy. -
Chronic Dysregulation:
If stress persists without recovery, the HPA axis can become dysfunctional, leading to either chronic high cortisol (affecting metabolic and immune function) or insufficient cortisol (leading to fatigue and poor stress response).
Chronic Stress and High Cortisol Leading to Leaky Gut:
High cortisol can affect gut health in multiple ways:
-
Increased Gut Permeability: High cortisol can compromise the integrity of the gut lining by increasing the expression of zonulin, a protein that regulates tight junctions between intestinal cells. When these tight junctions are weakened, the gut becomes more permeable, allowing toxins, undigested food particles, and pathogens to enter the bloodstream. This is commonly referred to as “leaky gut.”
-
Imbalance in Gut Microbiota: Chronic stress and elevated cortisol can lead to an imbalance in gut bacteria, favoring the growth of harmful bacteria and pathogens. This dysbiosis further impairs gut health and contributes to inflammation.
-
Increased Inflammation: Elevated cortisol over time can lead to systemic inflammation in the body. This inflammation can further exacerbate intestinal permeability and disrupt gut function.
Cortisol and Gut Health:
Cortisol, the body’s primary stress hormone, has a direct impact on gut health, and prolonged elevated cortisol levels due to chronic stress can contribute to leaky gut. Here’s how:
-
Disruption of the Gut Barrier:
- The gut lining, made up of epithelial cells, is held together by tight junctions. These tight junctions prevent harmful substances (like bacteria, toxins, and undigested food particles) from leaking into the bloodstream.
- Chronic elevated cortisol weakens the tight junctions between these cells, causing them to loosen and allowing particles to leak into the bloodstream. This condition is known as intestinal permeability or leaky gut.
-
Inflammation:
- Cortisol is released in response to stress and is designed to help the body manage acute stress. However, prolonged stress and continuous high levels of cortisol can lead to chronic inflammation.
- Chronic inflammation can damage the gut lining, impair digestion, and contribute to a dysregulated immune response. Inflammation can also increase the permeability of the gut, making it easier for harmful substances to enter the bloodstream.
-
Gut Microbiome Imbalance (Dysbiosis):
- Cortisol can influence the gut microbiome by encouraging the growth of harmful bacteria while suppressing beneficial ones. This creates an imbalance known as dysbiosis, which has been linked to leaky gut.
- Dysbiosis can further contribute to inflammation and immune activation, perpetuating the cycle of leaky gut.
-
Reduced Blood Flow to the Gut:
- During times of stress, cortisol increases sympathetic nervous system activity, which is responsible for the “fight or flight” response. This results in shunted blood flow away from the gut and toward the muscles and brain to prepare for physical activity.
- Reduced blood flow to the gut leads to poor digestion and compromised gut integrity, making it more prone to damage.
-
Altered Digestive Enzyme Production:
- Elevated cortisol levels can impact the production and secretion of digestive enzymes. This can impair the digestion of food, contributing to intestinal dysbiosis and gut irritation, both of which can lead to leaky gut.
Excessive Exercise and Leaky Gut:
Excessive exercise, especially in the form of high-intensity endurance training, can also contribute to leaky gut in several ways:
-
Increased Cortisol Production:
- Intense or prolonged physical exercise can lead to an increase in cortisol levels, especially when recovery is inadequate.
- The body uses cortisol to manage the physical stress of exercise. However, chronic high cortisol levels can cause the same gut-permeability issues as seen in chronic stress, damaging the gut lining and contributing to leaky gut.
-
Increased Intestinal Permeability:
- Research shows that endurance athletes and those who engage in intense physical activity may experience a temporary increase in gut permeability (leaky gut) during or after exercise. This is often referred to as exercise-induced gut permeability.
- During prolonged or high-intensity exercise, blood flow is redirected from the gut to the muscles, resulting in ischemia (lack of oxygen) and damage to the gut lining. This damage increases intestinal permeability, which can persist even after the exercise session has ended if recovery is inadequate.
-
Intestinal Ischemia and Hypoxia:
- During prolonged or intense exercise, especially at high intensities, gut hypoxia (low oxygen levels in the gut) can occur because of reduced blood flow. This deprives the intestinal cells of oxygen, causing cellular damage to the gut lining and contributing to leaky gut.
- The lack of oxygen to the cells can also impair the gut’s ability to maintain its structural integrity, leading to intestinal barrier dysfunction.
-
Inflammatory Cytokine Release:
- Intense exercise can trigger the release of pro-inflammatory cytokines (such as TNF-alpha, IL-6), which can compromise the gut barrier. Chronic inflammation resulting from excessive exercise can lead to leaky gut, similar to what happens in chronic stress.
- These cytokines can increase intestinal permeability by disrupting tight junction proteins, which are essential for maintaining the integrity of the gut lining.
-
Gut Microbiome Imbalance:
- Excessive exercise can negatively affect the gut microbiome, promoting the growth of harmful bacteria and reducing the diversity of beneficial gut bacteria.
- An imbalance in the gut microbiome (dysbiosis) is a significant contributor to leaky gut. This is particularly problematic in athletes who engage in long-duration or high-intensity training without proper rest, recovery, and nutrition.
-
Low-Grade Inflammation from Overtraining:
- Overtraining syndrome occurs when the body is unable to recover adequately from intense and frequent exercise sessions. This can lead to low-grade systemic inflammation, which is another factor that can damage the gut lining and increase intestinal permeability.
- Overtraining often leads to a state of chronic inflammation, which exacerbates leaky gut.
Connecting the Dots:
Both chronic stress (with high cortisol) and excessive exercise can result in leaky gut through a combination of increased cortisol production, reduced blood flow to the gut, increased inflammation, and damage to the gut lining. In both cases, managing stress levels, ensuring adequate recovery time, and maintaining a balanced diet to support gut health are crucial strategies to prevent leaky gut and its long-term effects on overall health.
Prevention and Recovery Strategies:
- Adaptogens: Such as ashwagandha and rhodiola can help reduce cortisol levels and combat the negative effects of stress and exercise-induced inflammation.
- Anti-inflammatory foods: Omega-3-rich foods (like fatty fish, walnuts, and flaxseeds) and antioxidants can help reduce inflammation and promote gut healing.
- Probiotics and Prebiotics: These can help restore the balance of the gut microbiome and support gut health.
- Adequate Rest and Recovery: For athletes, ensuring enough recovery time between intense workouts is key to preventing gut permeability and inflammation.
- Stress Management: Incorporating stress-reducing activities like meditation, yoga, and deep breathing exercises can help lower cortisol levels and protect gut health.
By addressing the causes of both chronic stress and excessive exercise, you can prevent and support the healing of leaky gut, thus protecting overall gut integrity and improving health.
Connection to Autoimmune Disease:
Leaky gut and chronic stress can contribute to the development or exacerbation of autoimmune diseases through molecular mimicry and increased systemic inflammation:
-
Molecular Mimicry: When the gut becomes permeable, harmful particles like pathogens or undigested food proteins can enter the bloodstream. The immune system may recognize these particles as foreign invaders and begin attacking them. If the particles resemble your body’s own tissues, the immune system may mistakenly attack healthy cells, contributing to autoimmune conditions (e.g., rheumatoid arthritis, Hashimoto’s thyroiditis, etc.).
-
Inflammation: Chronic stress and high cortisol can increase the production of pro-inflammatory cytokines. This systemic inflammation can trigger or worsen autoimmune conditions by heightening the immune response.
-
Immune System Dysregulation: High cortisol can impair the regulatory functions of the immune system, making it less able to differentiate between harmful and harmless substances. This can result in a misdirected immune response that attacks the body’s tissues.
In summary, chronic stress and high cortisol can lead to gut permeability, inflammation, and immune dysregulation, all of which contribute to the development or worsening of autoimmune diseases. Addressing the root causes of chronic stress, supporting adrenal function, and promoting gut health are critical for mitigating these effects.
In nutritional therapy, addressing chronic stress and imbalances in cortisol levels (either low or high) often involves providing the body with the necessary macronutrients and micronutrients that support adrenal health, regulate cortisol production, and help balance the effects of stress on the body. Here’s a breakdown of key nutrients that are involved in chronic stress and cortisol regulation:
Macronutrients: Proteins: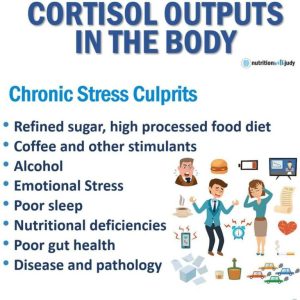
Amino Acids (especially Tyrosine and Tryptophan):
- Tyrosine: An amino acid that is crucial for the synthesis of dopamine, norepinephrine, and epinephrine, neurotransmitters that help manage stress and mood.
- Adequate levels of tyrosine are important for managing stress and maintaining cognitive function.
- Tryptophan: A precursor to serotonin, which helps regulate mood and stress levels. It also plays a role in the production of melatonin, promoting restful sleep, which is essential for managing cortisol levels.
- Cortisol Production and Protein: During times of chronic stress, the body may require more protein to produce sufficient amounts of cortisol. If protein intake is too low, the body may struggle to produce enough cortisol to respond to stress appropriately.
Carbohydrates:
- Complex Carbohydrates (Root Vegetables, etc.):
- Consuming complex carbohydrates helps stabilize blood sugar levels, which is particularly important in managing cortisol. Low blood sugar (hypoglycemia) can trigger an increase in cortisol production, exacerbating stress.
- Complex carbohydrates also stimulate serotonin production, helping to regulate mood and reduce the impact of stress.
- Balanced blood sugar levels help prevent the chronic spikes and crashes that can occur with high cortisol levels.
- Glycemic Control: Excessive intake of simple sugars can cause insulin resistance and increase cortisol levels. This makes it important to focus on nutrient-dense, whole-food sources of carbohydrates that don’t cause large fluctuations in blood sugar.
Fats:
- Healthy Fats (Omega-3 Fatty Acids):
- Omega-3s (from fatty fish like salmon, walnuts, and flaxseeds) play a vital role in reducing inflammation caused by chronic stress. Chronic stress tends to increase the production of pro-inflammatory cytokines, which omega-3s help to mitigate.
- Omega-3s also support brain health, improving mood and cognitive function, which can become compromised during prolonged stress.
- Cholesterol: Cholesterol is a precursor for the production of cortisol. Low cholesterol levels may impair cortisol synthesis, while adequate intake ensures the body can produce enough cortisol in response to stress.
Micronutrients:
B Vitamins:
- Vitamin B5 (Pantothenic Acid): This vitamin is crucial for adrenal function and cortisol production. It is often depleted during times of stress. Low levels can contribute to adrenal fatigue, characterized by low cortisol and symptoms like fatigue, irritability, and brain fog.
- Vitamin B6: Helps regulate the production of neurotransmitters such as serotonin and dopamine. B6 is also involved in the metabolism of proteins, carbohydrates, and fats and plays a key role in the stress response.
- Vitamin B12: Essential for the function of the nervous system and energy production. Stress can deplete vitamin B12 levels, leading to fatigue, mood imbalances, and cognitive dysfunction.
- Folate (B9): Important for the production of neurotransmitters, which regulate mood and stress responses. Folate works synergistically with B12 to support the nervous system and help with stress management.
Vitamin C:
- Antioxidant Role: Vitamin C is crucial for adrenal health as it helps regulate cortisol production. The adrenal glands have high concentrations of vitamin C, and it is used up during the production of cortisol.
- Immune System Support: Chronic stress can weaken the immune system, and vitamin C helps bolster the immune response and combat stress-induced inflammation.
Magnesium:
- Relaxation and Stress Response: Magnesium helps regulate cortisol and promotes relaxation by supporting the production of GABA (a calming neurotransmitter). It also helps with muscle relaxation and sleep, which are often disrupted during periods of high stress.
- Cortisol Regulation: Magnesium can help lower the excessive release of cortisol that occurs during stress and restore balance to the body’s stress response.
Zinc:
- Immune System Support: Zinc is important for the immune system and can help reduce inflammation. Chronic stress often leads to immune suppression, and adequate zinc can help prevent that.
- Cortisol and Stress Response: Zinc plays a role in regulating cortisol levels and supports adrenal health. Low levels of zinc are associated with impaired adrenal function, contributing to fatigue and difficulty handling stress.
Vitamin D:
- Immune Function: Low vitamin D levels have been linked to increased inflammation and an impaired immune response, which can be exacerbated by chronic stress.
- Mood Regulation: Vitamin D is involved in the production of neurotransmitters and hormones that affect mood and the stress response. Low levels can contribute to depression and heightened stress sensitivity.
Adaptogens (Herbal Supplements):
- Ashwagandha: Known for its ability to help reduce cortisol levels and enhance the body’s response to stress. It is particularly helpful for those with adrenal fatigue and chronic stress.
- Rhodiola: Another adaptogen that can help regulate cortisol production and reduce symptoms of mental fatigue and stress.
- Holy Basil (Tulsi): Helps manage cortisol levels and reduce inflammation linked to chronic stress.
Summary:
- In nutritional therapy, addressing chronic stress and cortisol imbalances involves ensuring adequate intake of both macronutrients (protein, complex carbohydrates, and healthy fats) and micronutrients (B vitamins, vitamin C, magnesium, zinc, vitamin D) that support adrenal health, cortisol regulation, and overall stress resilience.
- A nutrient-dense diet rich in these nutrients can help manage the effects of chronic stress, prevent insulin resistance, and promote better hormonal balance.
- Adaptogens like ashwagandha and rhodiola can also be supportive in regulating the stress response and balancing cortisol levels.

Chronic stress and high cortisol levels can significantly contribute to leaky gut (intestinal permeability) and increase the risk of autoimmune disease through several interconnected mechanisms.
1. Chronic Stress & High Cortisol → Leaky Gut
- Cortisol Dysregulation: When stress is chronic, cortisol remains elevated, leading to dysregulation of the immune system and increased inflammation.
- Disruption of Tight Junctions: The gut lining is protected by tight junctions between epithelial cells. Chronic stress increases zonulin, a protein that breaks down these tight junctions, allowing undigested food particles, toxins, and bacteria to enter the bloodstream.
- Decreased Mucosal Barrier: Stress reduces the production of secretory IgA (sIgA), an immune protein that protects the gut lining. Low sIgA increases susceptibility to gut dysbiosis and pathogenic bacteria overgrowth.
- Altered Gut Microbiome: Chronic stress shifts the gut microbiota, decreasing beneficial bacteria (e.g., Firmicutes and Bifidobacteria) and increasing pathogenic microbes, which can further damage the intestinal lining.
- Reduced Digestive Function: Stress diverts energy away from digestion, reducing stomach acid, bile flow, and enzyme production, which can lead to bacterial overgrowth (SIBO) and further gut inflammation.
If low cortisol (often seen in HPA axis dysfunction or adrenal insufficiency) is present, it can still contribute to leaky gut and autoimmune disease, but through slightly different mechanisms than high cortisol.
Low Cortisol → Leaky Gut
- Weakened Immune Regulation: Cortisol plays a role in modulating inflammation. When cortisol is low, the immune system can become hyperactive, leading to chronic low-grade inflammation in the gut lining.
- Increased Susceptibility to Gut Infections & Dysbiosis: Cortisol helps regulate gut microbiota by controlling inflammation. Low cortisol levels may allow pathogenic bacteria, yeast (e.g., Candida overgrowth), and parasites to thrive, further damaging the gut lining.
- Poor Mucosal Defense: Low cortisol is associated with reduced secretory IgA (sIgA), an important immune barrier in the gut. This weakens gut defense, increasing vulnerability to food sensitivities, toxins, and infections.
- Slow Gut Motility & SIBO: Low cortisol can contribute to slow gastric emptying and reduced gut motility, leading to small intestinal bacterial overgrowth (SIBO), which further increases inflammation and gut permeability.
Leaky Gut → Autoimmune Disease
With a compromised gut barrier, toxins, bacteria, and undigested proteins (like gluten and casein) leak into the bloodstream, triggering molecular mimicry, where the immune system mistakenly attacks self-tissues. This is a key driver of autoimmune diseases such as:
- Hashimoto’s Thyroiditis
- Rheumatoid Arthritis
- Lupus
- Celiac Disease

Endurance exercise, particularly when it’s prolonged and intense, can contribute to leaky gut through several interconnected mechanisms.
Here’s how it works:
-
Reduced Splanchnic Blood Flow (Ischemia):
- Mechanism: During prolonged exercise, blood is preferentially redirected to the working muscles. This diversion reduces blood flow (and oxygen) to the gastrointestinal (GI) tract, leading to ischemia (a state of reduced oxygen delivery).
- Impact: The intestinal cells, deprived of adequate oxygen, become stressed and can begin to malfunction.
-
Epithelial Damage & Tight Junction Disruption:
- Mechanism: The ischemic stress compromises the integrity of the intestinal epithelial cells. Specifically, the proteins that form the tight junctions (such as occludin and claudins) between cells become disrupted.
- Impact: This disruption creates gaps in the gut lining, allowing substances (like toxins, undigested food particles, and bacteria) to pass through into the bloodstream—a phenomenon known as leaky gut.
-
Reperfusion Injury & Oxidative Stress:

- Mechanism: When exercise ceases, blood flow returns to the gut (reperfusion). This sudden influx can generate reactive oxygen species (ROS), leading to oxidative stress.
- Impact: Oxidative stress further damages the already compromised epithelial cells and tight junctions, exacerbating intestinal permeability.
-
Inflammatory Cascade:
- Mechanism: The translocation of gut contents (like bacterial endotoxins) into the bloodstream triggers an immune response.
- Impact: This can lead to systemic inflammation, which may contribute to a chronic inflammatory state if exercise-induced gut permeability is a repeated event.
-
Mechanical Stress:
- Mechanism: In activities like running, the repetitive jostling and impact can add a mechanical strain on the GI tract.
- Impact: This physical stress further compromises gut barrier integrity, especially when combined with reduced blood flow and oxidative stress.
Key Takeaway
While endurance exercise is beneficial for overall health, excessive or improperly managed training can, through mechanisms like reduced blood flow, ischemia-reperfusion injury, and oxidative stress, compromise the gut barrier. This can lead to a leaky gut, allowing inflammatory triggers into the bloodstream, which may eventually contribute to systemic inflammation and other health issues.
By understanding these mechanisms, athletes and health optimizers can take steps (like proper hydration, nutrition, and recovery strategies) to mitigate these effects while still enjoying the benefits of endurance exercise.
Remember… Both high and low cortisol can contribute to leaky gut and autoimmunity, but in different ways:
- High cortisol → breaks down gut lining due to excessive inflammation & stress response.
- Low cortisol → weakens immune defenses, leading to infections, dysbiosis, and gut barrier dysfunction.
Supporting HPA axis balance, gut health, and immune modulation is key to preventing and managing these conditions
Balancing the HPA axis, supporting gut health, and modulating the immune system are key to preventing and managing leaky gut and autoimmune disease—whether cortisol is high or low. Here’s a targeted approach:
Support HPA Axis & Cortisol Balance
For High Cortisol:
- Adaptogens: Rhodiola, ashwagandha, holy basil (modulate stress response)
- Blood Sugar Stability: Avoid blood sugar crashes by eating protein + healthy fats with meals
- Circadian Rhythm Support:
- Morning sun exposure and movement
- Limit blue light at night
- Early bedtime (10-11 PM)
- Breathwork & Parasympathetic Activation: Daily deep breathing, meditation, vagus nerve exercises
For Low Cortisol:
- Hydration + Electrolytes: Sea salt, potassium, and magnesium support adrenal function
- Protein + Carbs in the Morning: Prevents hypoglycemia, which can stress the adrenals
- Adaptogens for Adrenal Support: Licorice root (for very low cortisol), ginseng
- Gentle Movement: Avoid high-intensity workouts; prioritize walking, yoga, strength training
Repair Gut Barrier (Leaky Gut Protocol)
- Remove Triggers:
- Processed foods, gluten, dairy (if sensitive), excess alcohol, artificial sweeteners
- Reduce gut infections (SIBO, Candida, H. pylori, parasites) via targeted antimicrobial protocols
- Rebuild Gut Lining:
- Collagen & Bone Broth: Support gut integrity
- L-Glutamine: Repairs intestinal lining
- Aloe Vera & DGL Licorice: Soothe gut inflammation
- Support Digestive Function:
- Digestive enzymes & HCl: If bloating and sluggish digestion are present
- Bitter herbs: Ginger, dandelion, apple cider vinegar
Restore Gut Microbiome
- Prebiotics & Fiber: Feed beneficial bacteria (onions, garlic, green bananas, resistant starch)
- Probiotics:
- Spore-based probiotics (MegaSporeBiotic, Just Thrive): Help repair gut lining
- Lactobacillus & Bifidobacteria strains: Support immune function
- Postbiotics (Butyrate): Helps reduce gut inflammation, especially if Firmicutes are low
Modulate the Immune System (Autoimmune Prevention)
- Vitamin D & Omega-3s: Regulate immune response and reduce inflammation
- Curcumin & Quercetin: Natural inflammation modulators
- Molecular Mimicry Awareness: If autoimmune conditions are suspected, test for gluten cross-reactivity (dairy, soy, corn)
- Cold Exposure & Sauna Therapy: May help regulate immune system response
Below is a sample protocol that we can fine-tune based on your lab results. Using markers from tests like the DUTCH test or an adrenal panel, we can identify whether your cortisol is high or low and then target the protocol accordingly.
Tailored Protocol for High Cortisol
Lab Markers to Look For:
- Elevated free cortisol levels (especially in the evening)
- A flattened diurnal rhythm (less of a drop at night)
- Signs of adrenal overactivity
Key Strategies for HIGH cortisol:
-
Stress Reduction & Lifestyle:
- Mindfulness & Meditation: Practice daily mindfulness, meditation, or deep breathing exercises.
- Sleep Hygiene: Prioritize a consistent sleep schedule with early bedtime, minimal blue light exposure at night, and a relaxing pre-sleep routine.
- Regular, Moderate Exercise: Engage in activities like walking, yoga, or light resistance training rather than high-intensity workouts.
-
Adaptogenic Support:
- Ashwagandha, Rhodiola, or Holy Basil: These help modulate the stress response and balance cortisol levels.
- Nutrient Support: Magnesium and B vitamins can support the nervous system and help manage cortisol spikes.
-
Nutritional & Gut Support:
- Anti-inflammatory Diet: Focus on whole, unprocessed foods, lean proteins, and healthy fats. Avoid sugar and refined carbohydrates that can spike cortisol.
- Gut Healing Protocol: Include gut-repair nutrients like L-glutamine, collagen, and bone broth. Identify and remove potential dietary triggers (gluten, dairy, etc.) if sensitivities are present.
- Probiotics & Prebiotics: Support a healthy gut microbiome which, in turn, can help modulate the stress response and inflammation.
-
Additional Measures:
- Breathwork & Vagus Nerve Stimulation: Practices like diaphragmatic breathing or even cold exposure (if tolerated) can help reset the stress response.
- Cognitive Behavioral Techniques: Working with a therapist or coach to manage stress and anxiety can be beneficial.
Tailored Protocol for Low Cortisol
Lab Markers to Look For:
- Lower-than-normal morning cortisol or overall cortisol output
- Signs of adrenal fatigue (potentially low DHEA)
- Possible blood sugar instability, which stresses the adrenals
Key Strategies for LOW cortisol
-
Nutritional Support & Lifestyle:
- Balanced Meals: Start your day with a protein and healthy fat-rich breakfast to stabilize blood sugar and support adrenal function.
- Hydration & Electrolytes: Ensure proper hydration and consider supplementation with natural sources of electrolytes (sea salt, potassium, magnesium).
- Gentle Exercise: Engage in light to moderate activities such as walking, restorative yoga, or tai chi to avoid overstressing the adrenals.
-
Adrenal-Supportive Supplements:
- Licorice Root & Ginseng: These can help boost adrenal function, particularly when cortisol is low.
- Vitamin C & B Vitamins: Both are critical for adrenal health; vitamin C is often depleted when cortisol is low, and B vitamins help with energy production.
- Adaptogens (Adjusted): While adaptogens like ashwagandha are helpful, dosing may differ—consultation for a personalized plan is key.
-
Gut Repair & Immune Support:
- Gut Barrier Healing: Use L-glutamine, collagen peptides, or bone broth to repair the intestinal lining.
- Probiotics: Consider a high-quality, broad-spectrum probiotic to rebalance gut flora. Spore-based probiotics can be particularly effective for gut barrier support.
- Avoid Inflammatory Foods: Even with low cortisol, reducing exposure to gut irritants (gluten, dairy, processed foods) is important to minimize inflammation and prevent further adrenal stress.
-
Lifestyle & Stress Management:
- Routine & Rest: Prioritize consistent routines and adequate rest to support overall HPA axis recovery.
- Gentle Stress-Relief Techniques: Techniques like guided imagery, progressive muscle relaxation, or short, frequent breaks during the day can help maintain low-stress levels.
Next Steps:
-
Review Your Lab Results:
- Compare cortisol patterns (morning, midday, and evening levels) along with other adrenal markers (DHEA, aldosterone if available).
- Evaluate gut health markers through tests (e.g., GI Map, food sensitivity panels) to see where intervention is most needed.
-
Customize Dosages & Timing:
- Based on your cortisol pattern, dosing of adaptogens or adrenal support supplements (e.g., licorice root for low cortisol) can be adjusted.
- Timing of meals, supplements, and stress management techniques should align with your natural rhythms.
-
Monitor & Adjust:
- Use follow-up labs and symptom tracking to determine the effectiveness of the interventions.
- Adjust the protocol as needed based on ongoing feedback from your body and lab markers.

Action Plan for Restoring HPA Axis Function and Addressing Metabolic Chaos
Goal: Rebalance the HPA axis, reduce chronic stress, restore cortisol levels, and address metabolic dysfunction by targeting underlying causes of stress and dysfunction.
Step One: Comprehensive Assessment
Actions:
- Functional Lab Testing: Run comprehensive functional tests to assess the status of cortisol levels, adrenal function, thyroid health, blood sugar regulation, and gut health.
- Cortisol Testing: Conduct salivary cortisol testing at different times throughout the day (morning, afternoon, evening) to track cortisol patterns.
- Comprehensive Hormone Panel: Assess DHEA, pregnenolone, estrogen, progesterone, and testosterone to identify potential imbalances caused by HPA axis dysfunction.
- Gut Health Testing: Run tests like the GI-MAP or comprehensive stool test to assess for gut dysbiosis, intestinal permeability (leaky gut), and inflammatory markers.
- Blood Sugar and Insulin Levels: Measure fasting blood sugar, insulin resistance, and HbA1c levels to evaluate the impact of cortisol on blood sugar regulation.
Outcome:
- Obtain a clear picture of the body’s current state of HPA axis function, metabolic health, and gut integrity.
Step Two: Targeted Nutrition Strategy
Actions:
- Adaptogen Support: Implement adaptogenic herbs (e.g., ashwagandha, rhodiola, holy basil) to support adrenal health and regulate cortisol levels. Use these in short-term bursts to prevent adrenal fatigue.
- Blood Sugar Regulation: Focus on foods that stabilize blood sugar and prevent spikes in cortisol:
- Complex carbohydrates: Prioritize whole grains (e.g., quinoa, sweet potatoes, legumes), fiber-rich vegetables, and low-glycemic fruits to prevent blood sugar swings.
- Protein: Ensure adequate protein intake with each meal to stabilize blood sugar and support muscle recovery (e.g., grass-fed meats, wild-caught fish, plant-based proteins).
- Healthy fats: Include omega-3 fatty acids (e.g., wild salmon, flax seeds, walnuts) to reduce inflammation and support brain health.
- Nutrient Density: Focus on foods rich in vitamins and minerals that support adrenal and immune health:
- Magnesium: Found in leafy greens, pumpkin seeds, almonds. It helps lower cortisol and reduce stress.
- Vitamin C: Included in citrus fruits, bell peppers, broccoli. Essential for adrenal function and balancing cortisol.
- B-vitamins: Found in whole grains, eggs, legumes, and green leafy vegetables. These support energy production and stress resilience.
- Zinc: Found in pumpkin seeds, beef, and chickpeas. Important for immune health and hormone regulation.
Outcome:
- Stabilized blood sugar and insulin levels, supporting adrenal health and reducing inflammation.
Step Three: Lifestyle Adjustments
Actions:
- Stress Management: Implement daily practices to lower chronic stress and regulate the HPA axis:
- Mindfulness meditation (10-15 minutes per day) to reduce cortisol.
- Breathing exercises (e.g., box breathing, 4-7-8 breathing) to activate the parasympathetic nervous system.
- Journaling or gratitude practices to help process emotions and lower stress.
- Sleep Hygiene: Focus on quality sleep to allow for proper cortisol rhythm:
- Set a consistent sleep schedule (7-9 hours per night).
- Create a bedtime routine to wind down (e.g., avoiding screens, dimming lights).
- Avoid stimulants (e.g., caffeine, alcohol) in the evening.
- Exercise Optimization: Modify exercise routines to prevent overtraining:
- Reduce intensity or frequency of endurance training if needed to support recovery.
- Incorporate low-intensity activities like yoga, walking, or swimming to support overall well-being without overloading the adrenal glands.
- Ensure adequate rest days and prioritize recovery to avoid further stress on the body.
Outcome:
- Reduced chronic stress, improved sleep quality, and balanced exercise intensity.
Step Four: Gut Health Restoration
Actions:
- Leaky Gut Repair:
- Introduce gut-healing supplements like L-glutamine, colostrum, bone broth, and digestive enzymes to support gut lining repair.
- Implement a low-inflammatory diet (e.g., eliminating processed foods, gluten, and dairy) to reduce gut permeability and improve digestion.
- Probiotics and Prebiotics:
- Add probiotic-rich foods (e.g., fermented vegetables, sauerkraut, kimchi, kefir) to support gut microbiome health.
- Ensure adequate intake of prebiotic fiber (e.g., onions, garlic, asparagus) to promote healthy gut flora and prevent dysbiosis.
- Anti-inflammatory Diet: Focus on anti-inflammatory foods to reduce overall inflammation and support gut healing:
- Incorporate turmeric, ginger, and omega-3-rich foods like wild salmon and flax seeds.
Outcome:
- Improved gut permeability, reduced inflammation, and restored digestive health.
Step Five: Monitoring and Adjustments
Actions:
- Regular Re-testing: Follow up with functional lab testing (e.g., cortisol testing, GI-MAP) every 3-6 months to assess progress and identify adjustments.
- Symptom Tracking: Use a health journal to track changes in energy levels, sleep, mood, weight, and digestive health.
- Adjust Protocols as Needed: Based on testing and symptom tracking, adjust diet, supplementation, and lifestyle modifications to continue supporting adrenal recovery, metabolic balance, and gut health.
Outcome:
- Ongoing assessment of progress and fine-tuning of the action plan to address any remaining dysfunctions.
Final Outcome: Restoring Homeostasis and Balance
By following this personalized action plan, the goal is to restore balance to the HPA axis, improve adrenal health, support gut healing, regulate blood sugar, and enhance metabolic function. Over time, these actions will address Metabolic Chaos, reduce inflammation, and help the body recover from the harmful effects of chronic stress. This holistic approach will allow the body to regain resilience, improve energy levels, and restore optimal functioning across all systems, from the inside out.
Discover the transformative power of Coach Debbie Potts!



